Published On June 18, 2018
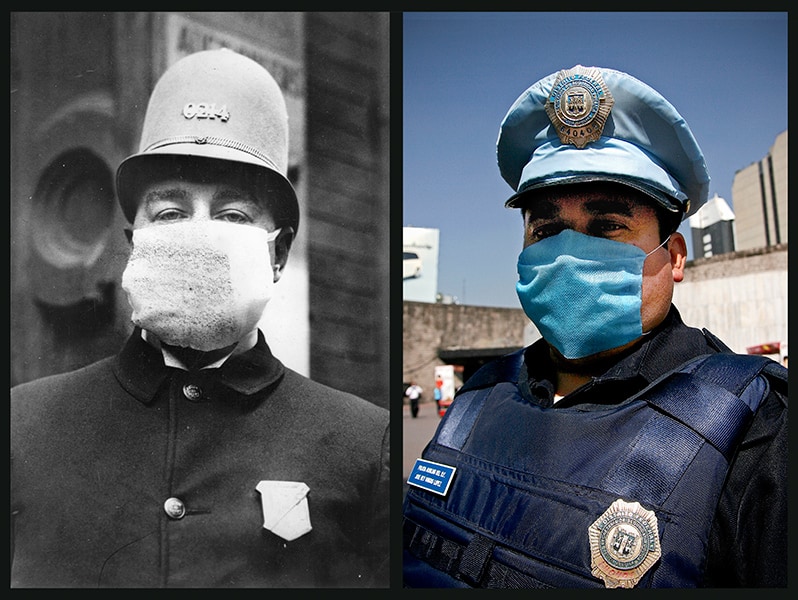
INFLUENZA VIRUSES CAUSE EPIDEMICS in the United States every year, year after year. Sometimes they are mild, with relatively few infections and low mortality. Other years they leave a deeper mark, as was the case this past winter, with news of overflowing intensive care units and of children who fell ill one day and perished the next. While infectious disease experts and others who study the flu are never certain of just how bad a season will be before it hits, they say that one thing is easier to predict: Some day, sooner or later, the world will likely face another serious pandemic—one that evokes the tragedy that struck in 1918.
The “Spanish flu”—misnamed, since no one is certain where it first struck, although many historians place its origins in Haskell County, Kansas—remains one of the worst known plagues in human history. When it arrived, the First World War had been raging for several years, building an international network of transmission routes. The war also put hundreds of thousands of soldiers in close, unsanitary conditions. By early spring, a strain of influenza virus began causing a number of deaths across the United States and other countries. The final estimated toll, when the disease had run its course in 1920, was between 50 million and 100 million people worldwide.
Medicine is better suited, in nearly every respect, to confront pandemics today. Seasonal flu vaccines are widely available; antibiotics can treat secondary bacterial infections, which were a major cause of deaths in 1918; and antivirals can both prevent the disease and control symptoms. Intensive care units provide life-saving technology that includes mechanical ventilators for damaged lungs, the lungs being where most secondary infections strike. Not least, epidemiologists can track the path and severity of an outbreak to help organize preventive efforts and treatment.
Yet there have been four pandemics since 1918, most recently in 2009, that have together killed more than 2.5 million people worldwide. A virus that carries the pathogenic punch of the 1918 influenza could still prove devastating, says virologist Jeffery K. Taubenberger of the National Institute of Allergy and Infectious Diseases (NIAID)—especially for people around the globe who lack access to advanced medical care. “Many would not be much better off than in 1918,” says Taubenberger, who believes another death toll of tens of millions would not be out of the question.
Flu viruses change frequently, and if a newly evolved virus is so unlike previous pathogens that humans have no preexisting immunity to it, the risk of a pandemic becomes especially great. On the lookout for such a virus, health officials are currently most concerned about the H7N9 avian virus, which originated in China in 2013 and has killed more than 600 people. In its current form, H7N9 virus doesn’t seem able to be readily transmitted among humans, but mutations could give it that ability. “If that happens, we would likely have a pandemic,” says Tim Uyeki, a medical epidemiologist in the influenza division of the Centers for Disease Control and Prevention. “That is what keeps me up at night—literally.”
The best solution for heading off a new pandemic would be a universal vaccine—one that protects against not only known variations on the flu virus but any new subtypes that might appear. Such a vaccine would also help with the scattershot protection offered by current flu shots, which are reformulated each year to protect against the strains that seem to pose the greatest danger. Today’s flu vaccines reduce the risk of developing the disease by, at most, 60%. In bad years, that advantage may drop to 10%.
Infectious disease experts emphasize that current influenza vaccines nonetheless offer crucial protection, especially by making the disease less toxic in people who become infected. A 2017 study found that unvaccinated flu patients in the hospital were two to five times more likely to die than those who had received flu shots. Still, today’s vaccines are routinely stymied by the flu virus’ uncanny ability to mutate, rearranging its genetic makeup in subtle and significant ways that help it hide from the immune system. The next generation of vaccines in development takes that shape-shifting into account and tries to find a way around it—by, among other methods, focusing the power of the immune system on parts of the virus that don’t change. The work carries a sense of urgency, taking place as it does under the specter of 1918 and the probability that an especially deadly flu season will yet again be upon us.

SCIENTISTS FIRST ISOLATED THE influenza virus in the early 1930s, more than a dozen years after the 1918 pandemic; a decade later the first flu vaccines became available in the United States. Each February, an advisory board at the Food and Drug Administration identifies the flu strains that are known to be circulating and selects which ones manufacturers should include in vaccines to be sold in the United States the following fall.
Most flu vaccine is still produced as it has been for 70 years—by slowly growing viruses in eggs, a complex, multistep process that takes about six months. By the time a batch of flu vaccine is ready—just in time for the U.S. flu season—the dominant strains in circulation may have changed. Flu viruses change frequently, and protein structures in the virus can subtly drift as it is passed from person to person. One of the key proteins that can change is the hemagglutinin, the structure the vaccine trains the immune system to guard against. If that structure has changed significantly, the vaccine becomes less effective. Moreover, viruses undergo mutations to survive and reproduce in eggs, and mounting research suggests that this phenomenon can play a significant role in spoiling the match between flu strains included in seasonal vaccines and the viruses in circulation.
To overcome the problem of mismatched vaccines, some researchers are looking at the “conserved” parts of the flu virus—the ones that generally don’t change. To understand this, consider that the flu virus is studded with mushroom-shaped surface proteins: hemagglutinin and another, called neuraminidase. The head portion of hemagglutinin attracts the most attention from the human immune system, which attacks it with proteins called antibodies to eradicate the virus. Hemagglutinin heads, however, also happen to be the sites of frequent antigenic changes, which create new strains the immune system doesn’t recognize. That helps explain why vaccines often fail to protect against the flu.
One potential solution, then, is to redirect the immune system’s attention from the head to the stalk, which doesn’t undergo these mutations, says microbiologist Peter Palese of the Icahn School of Medicine at Mount Sinai in New York City. Past attempts tried simply to chop off the heads and hope the immune system would refocus attention on the stalk. But headless stalks turned out to be too structurally unstable to be used in vaccines aimed at inducing protective antibodies.
Palese and his colleagues created a structure called a chimeric hemagglutinin (cHA), which tricked the immune system into making protective antibodies against the stalk as well as the conserved neuraminidase. They started with a virus that sickens humans, removed the hemagglutinin heads, and in their place fused on the heads of “exotic” hemagglutinins, borrowed from avian flu strains that are harmless to people. In animal studies, repeated inoculations with a cHA-based vaccine persuaded the immune system to ignore the strange head and instead to direct antibodies against the stalk and the neuraminidase, says microbiologist Florian Krammer, Palese’s colleague at Mount Sinai and a frequent co-investigator.
In theory, this kind of universal vaccine would train the immune system to recognize a portion of the virus that remains unchanged in all forms of influenza—both seasonal flu and any new, particularly virulent strains. So far, says Palese, the cHA-based vaccine has worked beautifully in mice and ferrets, protecting them against every strain of flu virus the research team has tried, including some from as early as 1934. “Our dream,” says Krammer, “is to be able to vaccinate kids twice, maybe three times, and have them never need another flu shot.” Two human trials, supported by pharmaceutical giant GSK and the Gates Foundation, are in progress.
Meanwhile, other groups are trying new ways to make vaccines with headless hemagglutinin. A team led by scientists at NIAID has made headless stalks more stable by anchoring them to the blood protein ferritin. With such a vaccine, the body detects the presence of hemagglutinin, and the immune system responds as it would to a real virus, says John Mascola, director of NIAID’s Vaccine Research Center. In a 2015 study published in Nature Medicine, Mascola and his colleagues reported that a vaccine made with headless hemagglutinin stalks protected mice and ferrets from a dose of H5N1 avian flu that was lethal to unvaccinated lab animals.
OTHER GROUPS ARE LOOKING past the virus’s heads and stalks. Microbiologist Ted M. Ross, director of the University of Georgia’s Center for Vaccines and Immunology, leads a team that hopes to achieve a universal vaccine by creating a comprehensive structure that contains every likely epitope in a single antigen. Ross developed a technique—computationally optimized broadly reactive antigen, or COBRA—that draws from databases of genetic data on hundreds of strains of influenza viruses that have been reported over the years. The goal is to identify the most dominant hemagglutinin epitopes—the parts of antigens that antibodies attack—and use their genetic sequences to create one encyclopedic synthetic molecule. This would then be introduced into the body, stimulating an immune response to all possible flu viruses—theoretically, even strains of the influenza viruses that don’t yet exist.
Ross and his colleagues have used a COBRA-derived vaccine to inoculate mice and ferrets against all strains of H1N1 and H3N2 flu—the viruses widely circulating now in people—as well as the H5N1 avian virus, which is rare but often deadly in humans. Ross says his experimental vaccines guard against 90% of all known strains, at least in animals. It remains to be seen how durable that protection will be, “but if it lasts for four or five years, that’s better than what we’re doing now,” says Ross. Drugmaker Sanofi Pasteur has licensed this technology, which is currently being developed for possible testing in humans.
Still other vaccine developers are looking beyond antibodies altogether, with the goal of stimulating a different mechanism of the human immune system. “There is a kind of hierarchy in the immune response,” says Tamar Ben-Yedidia, chief scientific officer of the biotechnology company BiondVax in Ness Ziona, Israel. B cells in the immune system generate the antibodies that often block a flu virus’s infection of a cell. But if antibodies fail, T cells confer another layer of protection, producing immune modulators called cytokines that directly attack infected cells and stop influenza from proliferating. Moreover, immunity based on T cells remains high after recovery from the flu, reducing the risk of reinfection, even by other subtypes of the disease.
There are limits to what T cells can do, however. The immunity they provide declines after each flu infection, until they are no longer at high enough levels to protect, says Sarah Gilbert, a vaccinologist at the University of Oxford and cofounder of biotech firm Vaccitech. Vaccitech and BiondVax are both developing vaccines designed to boost the T cell response against the influenza virus. In one trial, BiondVax’s vaccine, known as M-001, was given to elderly men and women before they received the traditional flu vaccine, improving their immune response. More intriguing, three years later the tests performed on stored blood taken from these men and women showed that antibodies spurred by the vaccine also neutralized the H3N2 virus that caused widespread illness in the 2014–2015 flu season, suggesting that the injection might guard against viruses that evolve and circulate in the future. BiondVax is now preparing phase 3 clinical trials.
Similarly, Taubenberger and his colleagues at NIAID have tested a vaccine cocktail containing hemagglutinins from four subtypes of avian influenza—H1 and H3, which are subtypes that have caused pandemics and annual epidemics in humans, and H5 and H7, from avian viruses that have also caused lethal infections. This not only protected mice from those flu subtypes but also from H2 viruses, H6 viruses and other influenza subtypes that were lethal to other animals. How could it protect against types not included in the vaccine? Taubenberger says that part of the explanation may be that their vaccine cocktail, which triggers production of protective antibodies, may also stimulate T cells.

DESPITE THE PROMISE OF these disparate approaches, a truly universal influenza vaccine is likely decades away, says Anthony Fauci, director of NIAID, which earlier this year unveiled a strategic plan for creating a safe and effective universal influenza vaccine. Still, Fauci believes that broadly effective vaccines that protect against more than one subtype of the flu could be available much sooner. “There is going to be universal flu vaccine 1.0, then 2.0 and so on,” says Fauci. “We’re not going to get the right answer the first time.”
Other researchers question whether there will ever be a single flu vaccine that can provide all or even most people with something approaching total immunity. One somewhat controversial theory holds that a person’s immune system may be “imprinted” by the first flu virus it encounters and then will primarily produce antibodies to that virus subtype, paying less attention to others. That hypothesis isn’t universally accepted, but if true, the immune systems of older people might be too rigid to respond to a universal vaccine. Very young people, in contrast, who have never been exposed to the flu, would have immunological clean slates and could be strong candidates. “With a universal vaccine you could conceivably produce generations of young people who might develop immunity to new flu strains and new pandemics,” says Taubenberger, “but this kind of approach might not help fiftysomethings like me.”
In the meantime, researchers continue to look for ways to make conventional flu protection more effective. “If you could narrow the window, then you could better match them to evolving strains of a virus,” says Uyeki.
That means moving away from egg-based vaccine production, says Andrew Pavia, chief of the division of infectious diseases at University of Utah Health, an academic health care system in Salt Lake City. One current vaccine, FluBlok, is cultivated in insect cells and can be ready in six to eight weeks. Although it’s FDA-approved for use only in those who have egg allergies, in a 2017 study FluBlok provided better flu protection than a standard flu shot. Pavia believes that wider use of adjuvants, added ingredients that increase the immune response to influenza, could help reduce the flu’s annual impact, too.
Emerging technology could also speed production of vaccines in the event of a pandemic. For example, genetic vaccines, such as DNA and mRNA, currently under investigation could be ready within a few months after the genome of a pandemic virus is sequenced, says Mascola. The vaccines that Mascola and his colleagues have tested contain only the genetic sequence for hemagglutinin and therefore don’t form a full virus. “Muscle cells take up the DNA and make part of the flu virus—for instance, just the hemagglutinin—and the body produces an immune response to that protein,” says Mascola. In a 2017 study by NIAID scientists, 30 healthy adults were vaccinated with an H7 DNA vaccine, an inactivated H7N9 vaccine prime, or both. In the study, most of the participants who received the priming H7 DNA vaccine had at least a fourfold increase in antibodies against the H7N9 virus, compared with those who received only the H7N9 vaccine.
Creating better flu vaccines will require not only patience but a knowledge of history, says Taubenberger. It would be a mistake to believe that the terrifying virulence of the 1918 pandemic was an outlier caused by strange mutations in the virus that are unlikely to recur. “There are other viruses out there in the wild that share those features,” says Taubenberger. “Something like this could happen again.”

Dossier
“Reconstruction of the 1918 Influenza Virus: Unexpected Rewards from the Past,” by Jeffery K. Taubenberger et al., mbio, September 2012. This article explores how reassembling the 1918 flu has led to insights about influenza virus biology and pathogenesis.
“Chasing Seasonal Influenza—The Need for a Universal Influenza Vaccine,” by Catherine I. Paules et al., The New England Journal of Medicine, Jan. 4, 2018. This article outlines why the world needs a broadly effective flu vaccine, and why everyone should still get the current imperfect version.
The Great Influenza: The Story of the Deadliest Pandemic in History, by John M. Barry (Penguin Books, 2004). This heavily researched narrative chronicles the 1918 influenza pandemic and the first “great collision between nature and modern science.”
Stay on the frontiers of medicine
Related Stories
- Avian Flu, One Year Later
After the panic, the author of our article on avian flu discusses developments in the story.
- Fearing the Flu
The avian virus incubating in Asia is remarkably virulent. But nature itself may prevent a human pandemic.
- A Flu Scare, 10 Years Later
Infectious disease specialist Martin Hirsch looks at the worry over H5N1 and its aftermath.