Published On August 11, 2022
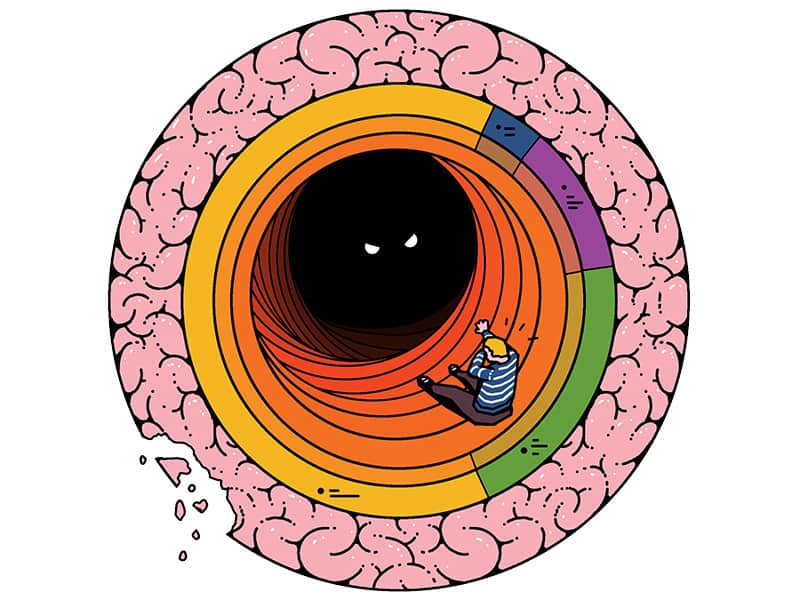
During his decades as Massachusetts General Hospital’s Chief of Psychiatry, Jerry Rosenbaum observed that patients suffering from a range of mental illnesses would sometimes get stuck in a state of rumination, or unceasing cycles of unpleasant, self-deprecating thoughts. While they had what were thought to be discrete conditions—depression, anxiety, addiction, obsessive-compulsive disorder—Rosenbaum wondered if the differences among those pathologies might be less important than the one characteristic that connected them. Finding ways to break the endless loops of rumination might lead to real progress, saving patients and their physicians from the difficult and sometimes futile quest to sort out which of the existing indicated therapeutic approaches might be effective for them.
Rosenbaum became fascinated with a 2018 neuroimaging presentation by Robin Carhart-Harris, a psychologist and then head of the Centre for Psychedelic Research at Imperial College London. It appeared to show similarities between brain areas affected by rumination and those acted upon by psychedelic drugs. Psychedelics seemed to decrease activity in the part of the brain known as the default mode network, possibly undercutting the process of rumination. “These drugs seem to work across an array of indications,” says Rosenbaum, who helped found and lead the new Center for the Neuroscience of Psychedelics at MGH. “There may be some broad, fundamental window that these drugs open that allows you to move from the state you’re in—which may be dysphoric or disabling—to one that is more freeing.”
That insight into how psychedelic compounds might actually operate on mental health represents a next step in a profound frontier. A resurgence of research into psychedelics—in new initiatives not only at MGH but also at Yale, Johns Hopkins, the University of California and the National Institutes of Health, among other places—is providing mounting evidence that the drugs might be effective alternatives for treating depression and other conditions. For optimal impact, and to minimize any danger to patients, researchers will need to figure out how they bring about their positive effects.

And the effects are sometimes extraordinary. In small trials, psilocybin, the most-studied psychedelic, has been shown to ameliorate tobacco addiction, alcohol addiction, obsessive-compulsive disorder, cancer-related anxiety and depression and treatment-resistant depression. Some patients who have taken the drug report feeling optimistic again after years of crippling depression that conventional treatments didn’t improve. Psilocybin is also being studied as a therapy for myriad other difficult-to-treat conditions, including methamphetamine use disorder, post-traumatic stress disorder, anorexia, fibromyalgia and phantom limb pain.
Yet the newness of this research, coupled with the difficulty of working with controlled substances, can make gathering insights much more difficult. In one recent psilocybin trial, for instance, patients who received the highest of three doses had a reduction in depression symptoms that lasted at least three months—a welcome development, says psychiatrist Sharmin Ghaznavi, associate director of the MGH Center for the Neuroscience of Psychedelics. Yet the data came from a phase 2 trial, with only 233 patients, and rolling the project out to a phase 3 deployment, which often enrolls thousands of research subjects, will pose a challenge. “Compared with how much clinical research data we have on other classes of drugs, these are early days,” says Ghaznavi.
Researchers will need to figure out how these drugs bring about their positive effects.
More data will be needed to answer the many open questions about how psychedelics work their profound effects in the brain. “I do think this is potentially one of the most important advances in psychiatry that I’ve seen in my career,” says Stephen Haggarty, who runs a chemical neurobiology lab in the MGH center. “But right now, from a fundamental neuroscience perspective, we understand so little.”
Through their work at the center, Rosenbaum, Ghaznavi, Haggarty and other researchers hope to elucidate what happens at molecular, cellular and network levels. If that picture becomes clearer, these researchers—and others around the world—might use this understanding to develop better, safer or more accessible substances or treatments. More immediately, uncovering the mechanisms of psychedelic drugs may show who exactly these drugs can help and in what contexts.
One day in 1943, a Swiss chemist studying ergot derivatives began to feel odd while working in his laboratory. Unsure what was happening, he abandoned his work for the day. “At home I lay down and sank into a not unpleasant intoxicated-like condition, characterized by an extremely stimulated imagination,” he wrote later. “In a dreamlike state, with eyes closed (I found the daylight to be unpleasantly glaring), I perceived an uninterrupted stream of fantastic pictures, extraordinary shapes with intense, kaleidoscopic play of colors.”
These psychoactive effects of the compound—lysergic acid diethylamide, or LSD—that Albert Hofmann had discovered were unintended. Yet Hofmann’s invention would help usher in a mid-1900s explosion of Western psychedelic research. In 1954, Aldous Huxley published The Doors of Perception, in which he documented his personal experiments with mescaline. Hofmann himself continued his research, and in 1958 he identified psilocybin as the active ingredient in “magic mushrooms,” a term coined a year earlier by Life magazine. In 1959, a closed conference at Princeton University addressed “the use of LSD in psychotherapy,” and the next year saw the first major European conference on psychedelics. During this period, hundreds of studies were published on the effects of psychedelics, including their use to treat addiction and other disorders.
Yet this period of scientific ferment ended almost as abruptly as it began. In 1961, psychiatrist Jonathan Cole, head of the Psychopharmacology Service Center at the National Institute of Mental Health and a pioneer in studying psychedelics, expressed “very mixed feelings” about the research, noting potential harms for patients. Experiments with psilocybin at Harvard University, some involving students, added to the negative image of the research, and psychedelics, especially LSD, came to be associated with the anti-war movement. LSD became illegal in the United States in 1968.
Interest in the therapeutic potential of the drugs came back slowly. The nonprofit Multidisciplinary Association for Psychedelic Studies was founded in 1986, and in 2000, researchers at Johns Hopkins were granted approval to study psychedelics—almost all of which today remain illegal, as Schedule 1 controlled substances. In 2006, those scientists published a landmark study showing that healthy volunteers experienced sustained “positive changes in attitudes and behavior” from single doses of psilocybin. Other research centers opened across Europe and North America, and public awareness and perception of psychedelics shifted favorably, aided in part by books such as Ayelet Waldman’s A Really Good Day (2017), about the author’s experiences with microdosing—taking very low doses that don’t trigger full hallucinations but may have beneficial effects—and Michael Pollan’s How to Change Your Mind (2018), in which the respected science journalist not only traces the history of psychedelics use and research but also details his own experiences with the drugs.
Classic psychedelics include drugs such as mescaline, psilocybin, LSD and DMT that appear to exert their effects primarily by binding to the 5-HT2A receptor in the brain, which normally responds to the neurotransmitter serotonin. (Ketamine and MDMA, which also have psychedelic properties, have different mechanisms of action.) The drugs’ subjective effects vary widely depending on who is taking them and the environment in which they’re taken. Some users experience changes in visual perception as well as how they perceive time and their own bodies. Other effects include feelings of awe and peace as well as spiritual or mystical experiences. Some users describe losing their sense of self and feeling unity with the greater world. Other users have a negative episode, or “bad trip,” which can also leave a lasting mark.
In one current frontier of psychedelic research, teams are working out what happens when 5-HT2A receptors are activated by psychedelics. Psychedelics seem to alter brain activity and connections among areas that are important for perception (including the visual cortex and the thalamus) and the prefrontal cortex, involved in cognition and self-referential thought, as well as altering communication between large-scale brain networks.
A related question is how those neurobiological reactions sometimes translate into long-term changes in well-being. Drugs such as psilocybin get washed out of the body rather quickly, notes Alex Kwan, an associate professor of neuroscience at Yale University. “One of the most important mysteries about these compounds is that while the ‘trip’ lasts only three or four hours in humans, there seem to be effects that can persist weeks or even months,” Kwan says. That’s in contrast to selective serotonin reuptake inhibitors (SSRIs) and other drugs for mental illness that have to be taken every day.
One potential explanation, says Kwan, is that psychedelics enhance neuroplasticity—the ability of neurons to make or strengthen new connections. There is a large body of evidence in both animal models and in people suggesting that chronic stress and depression are associated with reductions in plasticity and loss of synapses. But a single dose of psychedelics can kickstart plasticity at the cellular level. Kwan’s work has shown that within 24 hours of receiving psilocybin, mice had significant increases in the density of dendritic spines, tiny cellular projections that neurons use to gather incoming signals from other neurons. This increased spine density was still apparent one month later, indicating that a single short exposure may produce long-lasting changes in the brain.
LSD and DMT also promote neuroplasticity, and researchers are beginning to elucidate which genes and proteins are involved in 5-HT2A-mediated neuroplasticity. Expression of one of those proteins, brain-derived neurotrophic factor (BDNF), increases after a single dose of a psychedelic and results in greater dendritic complexity, a change that outlasts the acute effects of the drugs. In animal trials, repeated administration of a psychedelic was shown to stimulate creation of new neurons and increased BDNF levels for as long as a month after treatment.
Human imaging studies also enable scientists to observe changes in brain activity in real time, another avenue into understanding psychedelics’ dramatic effects. One hypothesis has been that, beyond promoting plasticity, short-term changes in brain activity and connectivity during a psychedelic trip could serve a sort of “reset” function, allowing people to break out of rumination and other pathological patterns of thought or behavior. The research on the default mode network that Jerry Rosenbaum found so intriguing suggests that normal activity and integration in that network seems to be reduced during a psychedelic experience and increased afterward. Perhaps this allows the brain to shake off bad habits and then function in a more normal way after treatment.
Changes in other brain networks could also be important. Psychedelics alter connectivity within feedback loops that run from the cortex to the striatum to the thalamus, and back to the cortex (the CSTC feedback loops). The effects in this network could explain some long-term benefits of psychedelics, says Manoj Doss, a researcher at the Johns Hopkins Center for Psychedelic & Consciousness Research. Doss notes that the striatum may be home to ingrained patterns of thought and behavior, and that it is involved in patterns of motor function and reward that go awry in addiction. “Altering this circuit with psychedelics might allow the rewriting of crystallized, automatic, maladaptive behaviors such as those in addiction or even depression,” Doss says.
Tripping on psilocybin or other drugs also produces thoughts and emotions in the conscious mind, and some—but not all—researchers believe this is crucial in explaining the long-term benefits psychedelics often seem to have. “It strikes me as pretty implausible that effects lasting months or even years could be explained solely by changes to neuroplasticity,” says David Yaden, an assistant professor at the Johns Hopkins Center for Psychedelic & Consciousness Research. Long-lasting changes must require cognitive alterations of some kind, he says, including “shifts in the way you view yourself, other people or the world as a whole.”
“There’s a lot of power in the psychedelic experience,” agrees Natasha Mason, a psychopharmacologist at Maastricht University in the Netherlands. “It gives patients agency and a lot more control over their healing, compared with just having a therapist tell them how they need to change. Psychedelics allow them to have their own insights.”
Indeed, multiple studies have shown correlations between subjective experiences during a trip and long-term benefits. As Yaden notes in a 2020 review paper, people who score higher on the Mystical Experience Questionnaire—which seeks to measure feelings of unity, sacredness, truth and transcendence—have greater reductions in tobacco cravings and symptoms of anxiety and depression. Participants in other studies reported that taking psychedelics gave them important insights into themselves and their problematic behaviors. Clinical psychologist and researcher Peter Hendricks at the University of Alabama at Birmingham proposed in 2018 that feelings of awe during a psychedelic experience may be a key part of the long-term changes in well-being and openness that many people report.
In an ongoing study, Christopher Nicholas, a clinical psychologist at the University of Wisconsin, is testing the insights-drive-change hypothesis in a novel way. His team is giving healthy volunteers psychedelics along with a dose of midazolam, a drug that relieves anxiety and also causes amnesia. His trial subjects have a psychedelic experience, but are not likely to remember it. That could help answer the question of the relative importance of neurobiological effects compared to subjective factors related to insight and emotional processes. If the volunteers show the improvements in mental health that psychedelics often produce but don’t have any memory of the experience, Nicholas says, then that could suggest that much of the change is driven by the drug’s psychopharmacological properties.
A separate frontier is looking at how to conduct this new generation of psychedelic research safely and effectively. One perplexing problem is how to conduct placebo-controlled trials. It’s easy for patients (and the clinicians monitoring them) to tell the difference between a drug that causes major alterations in cognition, emotion and perception and a placebo that doesn’t.
Another issue is patient safety, especially the need to avoid harm to trial participants who may have bad trips. In a survey of nearly 2,000 recreational psychedelic users, some 40% reported their worst trip to be one of the most challenging experiences of their lives, 11% put themselves or others in danger and 7% sought treatment for ongoing psychological problems afterward. To manage the serious risks associated with taking psychedelics, researchers must conduct studies in tightly controlled settings with substantial therapeutic support. At a minimum, says Sharmin Ghaznavi at MGH, patients need specially trained therapists to prepare them for the experience and to guide them through it and help them cope with any distress. They also need help afterward processing what happened to them. Sessions can take as long as eight hours, and researchers don’t yet know how often the process may need to be repeated. All of this makes psychedelic therapy resource-intensive, and if ongoing research confirms its effectiveness in treating a range of disorders, it could be challenging to make it widely accessible.
Patients need specially trained therapists to prepare them for the experience.
Many researchers are now exploring ways to increase accessibility. A non-hallucinogenic psychedelic, if proved to be effective, might reduce the need for supervision, and psychedelic-assisted group therapy could enable therapists to treat larger numbers of patients. Psychedelics that produce a shorter “trip,” such as 5-MeO-DMT, might also help.
Those and other issues will have to be addressed as the scientific understanding unfolds. “I think we’re still in the first inning here,” says Haggarty. “How do we make these agents safer? How do we think about a second generation of these drugs? How do we bring the concept of precision medicine into this—treating the right patient at the right time with the right drug?”
In addition to gathering more data, researchers also emphasize the need for accepting nuance and complexity. David Yaden at Hopkins says that in recent years the pendulum of public opinion has swung from overly negative, alarmist views on psychedelics to unrealistically positive expectations.
“It appears that there’s genuine promise for psychedelics to be effective treatments for some mental disorders,” he says. “Our society, all of us, have a role to play in this—to think critically about the evidence for psychedelics in a balanced way. And to avoid the temptation to fall into one extreme or the other.”
Dossier
“The Subjective Effects of Psychedelics Are Necessary for Their Enduring Therapeutic Effects,” by David B. Yaden et al., ACS Pharmacology & Translational Science, December 2020. The authors discuss the evidence for subjective effects relating to thoughts and emotions as an important mediator for the long-term, beneficial effects of psychedelics.
“Psychedelics and Neuroplasticity: A Systematic Review Unraveling the Biological Underpinnings of Psychedelics,” by Cato M.H. de Vos et al., Frontiers in Psychiatry, September 2021. This paper provides an overview of neurobiological changes engendered by psychedelics at the cellular and molecular level and highlights areas for future research.
Stay on the frontiers of medicine
Related Stories
- The Road to Functional Neurological Disorder
Once regarded as a purely mental condition, functional neurological disorder emerges from the shadows.
- The Mourning After COVID-19
Some people who lose loved ones to COVID-19 will face an inconsolable grief—a second epidemic the nation is poorly prepared to handle.
- How Do You Measure Mindfulness?
A calmer brain can lead to a healthier body. Researchers are beginning to pinpoint just where those benefits are coming from.