Published On January 22, 2019
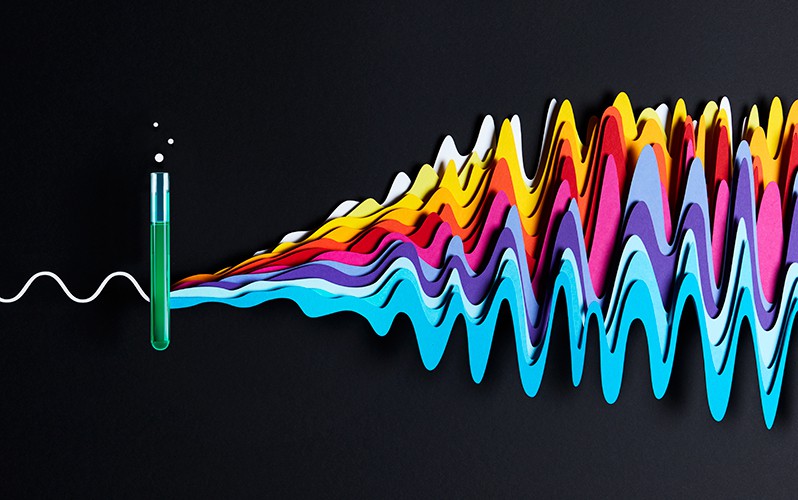
THE SENSATION OF SOUND, like all phenomena that make up the human experience, depends on an intricate relay of biological cells and signals running between the outside world and the brain. Human hearing begins when sound waves enter the outer ear and travel to the eardrum. There, sound waves are converted into vibrations and funneled to tiny bones in the middle ear, which amplify the vibrations and send them into the cochlea, a fluid-filled structure that resembles a snail shell. As the fluid in the cochlea vibrates, pressure variations move an internal membrane studded with bristly hair-like tufts, which belong to remarkable “hair cells” that can translate motion into an electric signal that runs along the auditory nerve to the brain.
Every step in this process plays out millions of times as people navigate the noise of daily life. But the modern world is much louder than the one of our human ancestors, and over decades, the many moving parts along the path from ear to brain may become damaged and deteriorate. Some 466 million people worldwide, and more than 37 million in the United States, have lost part or all of their ability to hear. Roughly one in three adults between ages 65 and 74 is affected, as are half of those over 75, and one in five veterans of the wars in Iraq and Afghanistan has lost some ability to hear because of bomb blasts and other battlefield noises.
While some lose their hearing because of exposure to loud noises, others are affected by faulty genes, head trauma, a mother’s infection during pregnancy or complications after birth. About three out of every 1,000 U.S. children are born with a detectable level of hearing loss, and some children who can’t hear well during infancy may not achieve functional speech and language, because the first two years of life are particularly important for developing communication skills.
With no single cause of hearing loss, no current approach can treat everyone, and even the most successful interventions have problems. Conventional hearing aids, for example, can help many people, yet they’re used by just one in five who might benefit, says Brad Welling, a neurotologic surgeon and chief of otolaryngology at Massachusetts General Hospital and Massachusetts Eye and Ear. They’re often rejected because they increase the volume of sounds but fail to convey clarity, making it difficult to distinguish speech from background noise.
Cochlear implants, considered miraculous when they were introduced in the mid-1980s, are the primary option for people who are profoundly deaf. These devices bypass damage in the ear itself and directly stimulate nerves in the inner ear. Yet cochlear implants are worse than hearing aids in their ability to provide anything close to natural hearing. They generate a digital sound within a very limited range of frequencies, fail in noisy environments and can’t help people properly hear music or other complex sounds. For some people, including those whose cochlear nerve is damaged or missing, the devices are no help at all.
Recent advances offer some improvement, with researchers approaching the problem along several fronts. They continue to expand what they know about the basic biology of hearing and how hearing loss develops in the hopes of finding new ways to repair and strengthen the signal as it travels to the brain. Gene therapy and CRISPR genome editing, so promising in other fields, may hold the key for treating genetic forms of hearing loss, and new kinds of drugs, as well as treatments involving stem cells, may regenerate or repair hair cells and nerves. Together, they offer hope that an epidemic of hearing loss may be coming closer to effective treatment.
THE BIOLOGICAL PROCESS OF hearing is still being decoded, step by step. For example, while researchers have known since the 1970s that hair cells transmit sound with the help of a crucial protein, it wasn’t until 2018 that they were finally able to identify that protein with certainty. In a paper published in Neuron, co-senior authors David Corey, professor of neurobiology at Harvard Medical School, and Jeffrey Holt, professor of otolaryngology and neurology at Harvard Medical School, showed that transmembrane channel-like 1 (TMC1), a protein discovered in 2002, is what converts sound vibrations into the electrical signals to the brain. What’s more, says Holt, “we think this protein underlies hearing in all vertebrates.”
Mutations in the gene TMC1, which produces the protein, are responsible for several kinds of genetic hearing problems and loss, says Holt. While the study focused on a basic science question, “TMC1 is interesting from a therapeutic perspective as well,” he says. Holt’s lab has been studying mice that are deaf because they lack functional TMC1, mimicking a form of human deafness. The researchers have been able to use gene therapy to reintroduce a functioning version of the TMC1 gene into the mice’s ears—a solution that has been quite effective, says Holt. “We can restore the ability of cells to convert sound waves into electrical signals,” he says.
This kind of gene therapy typically utilizes a virus or other vector to infect a cell and deliver a working copy of the target gene, with the vector modified so that it won’t cause disease or other unintended harm. But delivering it effectively to the ear, and in fact to most places in the body, remains a work in progress. For instance, adeno-associated viruses (AAVs) have often been tried as vectors, but because AAVs are quite common, the immune system tends to recognize and destroy them before they can carry their genetic cargo into the right place.
Luk Vandenberghe, director of the Grousbeck Gene Therapy Center at Mass. Eye and Ear, set out to generate a kind of AAV that would escape detection by the immune system while retaining the mechanical properties that make AAVs appealing. To do that he sought to recreate ancestral forms of the virus, using computational tools to predict how their structures may have evolved and reconstructing earlier generations. The most remarkable upshot of that work may be an AAV called Anc80, which has transferred genes efficiently to the cochlea in mice. “The ability of this virus to target the outer, in addition to the inner, hair cell in the cochlea is unique,” says Vandenberghe. That particular landing spot is important because the outer hair cell senses sounds and amplifies them, helping people distinguish very soft sounds and to focus their hearing in noisy, complex environments, such as a loud party.
Vandenberghe is a founder of Akouos, a biotech startup working on gene therapy treatments for patients with genetic hearing loss. His approach is similar to a pioneering gene therapy from Spark Therapeutics that was approved last year by the U.S. Food and Drug Administration to treat another kind of sensory disorder, a rare inherited form of blindness.
Gwenaëlle Géléoc, a researcher in neurobiology and otolaryngology at Boston Children’s Hospital, recently explored the Anc80 vector as a therapy for Usher syndrome, a devastating genetic disorder that causes profound deafness and blindness as well as balance issues. The results in mouse models were striking. The balance of the animals was restored and formerly deaf mice could hear sounds as soft as a whisper. The damaged hair cells in the mutant mice were repaired by the gene therapy, and their hair bundle structures became similar to those of normal mice. “Our results were very visual,” says Géléoc. “Mice with the Usher syndrome mutation would twirl and circle really heavily because of their balance defect. But the treated mice did not circle at all.”
In a related approach, David Liu, a chemical biologist at the Broad Institute of MIT and Harvard, and Zheng-Yi Chen, a researcher at Mass. Eye and Ear, have used a version of CRISPR-Cas9, a genome-editing system, to alter the genetic mutation in the TMC1 gene that causes progressive genetic hearing loss in humans. In CRISPR, a piece of RNA ushers an enzyme (Cas9) to the proper location in the genome, where it cuts out the mutated part of the target gene. Liu, Chen and their colleagues encapsulated these two pieces inside fatty molecules called lipids that are able to cross cell membranes. When they injected the lipid particles directly into the cochleae of the mice, the hair cells took up the lipids, and the Cas9 enzyme stripped out the mutated copy of the gene, improving the hearing of the mice.

NOT ALL FORMS OF hearing loss are natural targets for gene therapy or genome editing. The most common type of acquired hearing loss—sensorineural, which encompasses a range of afflictions to the inner ear and auditory nerves—is often brought on or made worse by environmental and lifestyle factors.
The conventional wisdom has been that acquired sensorineural hearing loss is largely caused by the gradual degeneration of cochlear hair cells, which aren’t replaced when they die. “One reason we’ve focused on hair cells is that there is really clear evidence for their demise,” says Sharon Kujawa, director of audiology research at Mass. Eye and Ear. Once people start to lose outer hair cells, their threshold for hearing increases—meaning that sounds must be made louder to be detected. That’s a change that can be charted on a hearing test audiogram, which shows the limits of pitch and volume that a person can hear in each ear.
Yet many cases of hearing loss follow a different pattern. Patients complain of not being able to understand speech in difficult listening conditions, yet their audiograms indicate they are hearing sounds at a perfectly normal level. Research by Kujawa and Charles Liberman, who directs a series of labs dedicated to the study of hearing and deafness at Mass. Eye and Ear, may help explain this disorder. Kujawa was studying mice exposed to loud noise early in life that seemed to recover from the damage it caused—their audiogram thresholds were normal. But when the mice aged, the researchers noticed a “massive neural loss.”
It turned out the early noise had hurt the synapses that connect inner hair cells to the cochlear neurons. “That happened almost immediately after noise exposure,” says Kujawa. Up to half of the synapses were silenced, even while hair cells remained intact. Over time, the cell bodies of the neurons also died. “We’ve seen this in every animal model we’ve studied, in terms of noise exposure and age-related hearing loss,” she says.
This phenomenon—cochlear synaptopathy—has also been dubbed “hidden hearing loss” because it doesn’t show up on audiograms until roughly 80% of neurons are gone. And although the synaptic connections between cochlear neurons and hair cells may be destroyed immediately when they’re exposed to loud sounds, other parts of the nerve cells often survive for years or even decades. Kujawa doesn’t yet know how widespread this phenomenon is in humans, but it could be a major factor in age-related and noise-related hearing loss. A recent study from Liberman confirms evidence in humans of this synaptic decline.
Because parts of the cochlear sensory neurons survive for years, there appears to be a long therapeutic window for treating the lost connections. Liberman is studying one potential therapy involving neurotrophin-3, part of a family of proteins that help neurons develop, grow and survive. His work in mice has shown that neurotrophin-3 can be delivered directly to the inner ear via a gel placed on the “round window,” a membranous connection between the middle and inner ear. The treatment has regenerated hair cell synapses and restored neural function after noise exposure.
David Jung, an otolaryngologist and neurotologist at Mass. Eye and Ear, has taken Liberman’s approach a step further. He worked with Michael McKenna, a neurotologist at MGH, to develop a way to deliver a drug called bisphosphonate to the inner ear without damaging hearing. Bisphosphonate is currently under investigation as a way to treat a common inner ear disorder called cochlear otosclerosis. Jung then wondered whether he could attach a drug, such as a neurotrophin, to a bisphosphonate molecule and deliver this combined therapy to the bone of the cochlea—since bisphosphonate binds to bone with high-affinity—to help restore destroyed synapses. This “hybrid molecule” approach, still being studied, could perhaps be used to deliver other treatments to the cochlea.
Lost synapses may cause some age- and noise-related hearing loss, but hair cells themselves also die, and efforts to replace or regenerate them are another urgent line of investigation. One possible route is the use of stem cells. Researchers have been studying how hair cells develop in an embryo to better understand the “recipe” for coaxing stem cells to become hair cells—allowing them to make what are essentially hair cells in a dish. If they are able to master that, they might then get those cells to develop and function in a human inner ear.
Albert Edge, director of the Tillotson Cell Biology Unit at Mass. Eye and Ear, began working with just a few stem cells isolated from the cochleae of mice and has been developing drugs to stimulate gene expression and molecular signals that can push these dormant stem cells to become new hair cells. Thus far, his recipe is working well, and Edge and his team have created mature, functional mouse hair cells. Karl Koehler, assistant professor of otolaryngology at Indiana University School of Medicine, has been working along similar lines and has created an entire “inner ear in a dish” that includes vestibular hair cells, responsible for balance, as well as inner ear neurons. This organoid could be used to help understand the connections between various parts of the inner ear, such as the synapses between hair cells and neurons. It could also be used to test gene therapy, drug treatments and other potential therapies for hearing loss.
The understanding of why and how hearing loss happens has made great advances in recent years. But it has become even more clear that the causes are just that—causes, plural. “We know that hearing loss is really heterogeneous, and there won’t be one approach that helps almost everyone,” says Sharon Kujawa of Mass. Eye and Ear. “That’s the exciting part of all this—we’re beginning to see how to translate some of this research. A lot of people are working on different approaches because everybody sees a different part of the elephant—but in the end, all of those different things being studied happen in the ear, and in the brain, and in the whole person—and they do all have to be addressed.”
Dossier
“TMC1 Forms the Pore of Mechanosensory Transduction Channels in Vertebrate Inner Ear Hair Cells,” by Bifend Pan et al., Neuron, August 2018. This study provides evidence that the TMC1 protein is a significant factor in the process of transduction, whereby vibrations become electrical signals that are carried to the brain.
“Cochlear Synaptopathy in Acquired Sensorineural Hearing Loss: Manifestations and Mechanisms,” by M. Charles Liberman and Sharon G. Kujawa, Hearing Research, June 2017. This review of research on acquired sensorineural hearing loss demonstrates how ears exposed to loud noises show “exaggerated synaptic and neural losses” as they age.
“Treatment of Autosomal Dominant Hearing Loss by In Vivo Delivery of Genome Editing Agents,” by Xue Gao et al., Nature, January 2018. Researchers use a genome-editing approach to ameliorate hearing loss in a mouse model of genetic hearing loss.
Stay on the frontiers of medicine
Related Stories
- How a Sea Anemone Can Help Us Hear
A new way to understand and treat hearing loss comes from the deep waters of comparative biology.
- The Blind Can See
Stem cells, gene therapy and devices that can beam images directly into the brain offer new hope to those without sight.
- The Other Stem Cells
Once considered mere substitutes for embryonic cells, re-engineered adult cells are making breakthroughs of their own.