Published On March 15, 2018
SLEEP IS A TIME-TESTED CURE. It repairs damaged tissues, allows critical immune function to take place and encodes the day’s memories more deeply in the brain. But good sleep often deteriorates with age, and can also be thrown off by a number of medical conditions.
Improve the quality of sleep, and you have healthier people. But attempting to do that has mostly been a process of removing obstacles—clearing the airways, or reducing intake of caffeine and alcohol. Very little has been done to find treatments that would actively promote higher-quality rest.
One promising therapy, counterintuitively, involves subjecting a sleeper to a series of barely audible noises. These encourage patterns exhibited in the most restorative periods of sleep, say its adherents. The approach is called acoustic stimulation, and makes use of a type of brain wave called a K-complex.
In the 1930s, Harvard scientists, working in the private laboratory of financier Alfred Loomis, were looking at a sleeper’s EEG (electroencephalogram) recording and observed this distinctive wave form:
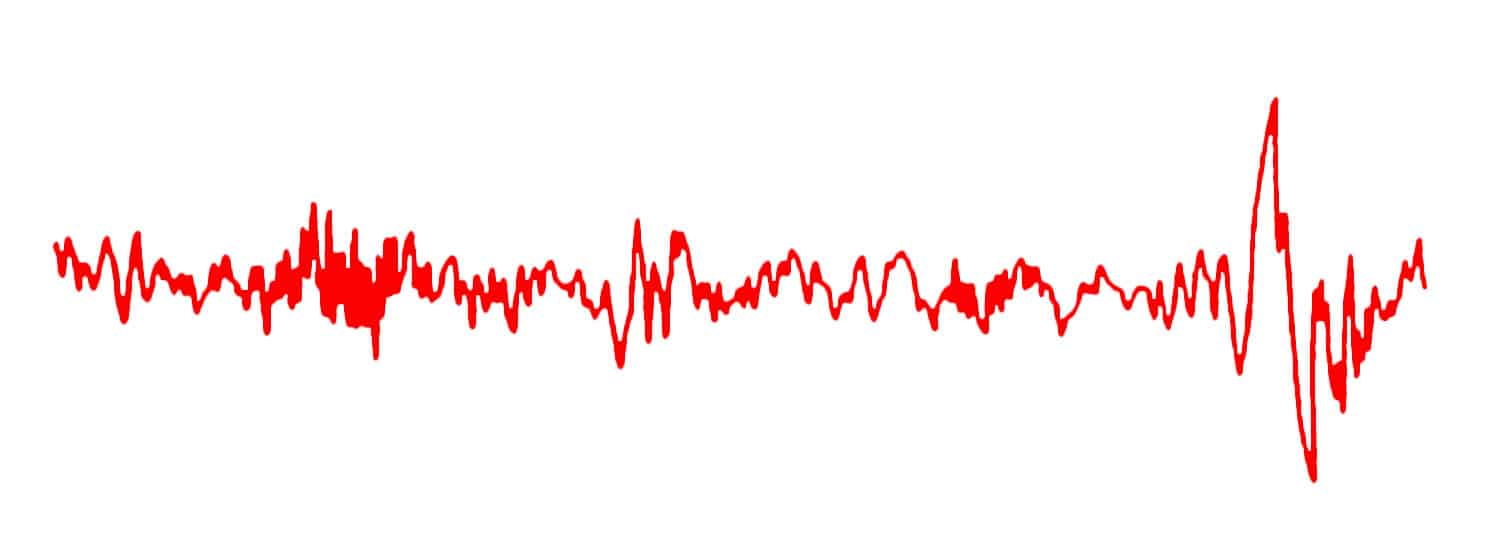
The so-called K-complex—a single high-amplitude wave—occurred naturally, but it could also be made to appear whenever someone touched the sleeper’s skin or made a soft noise. Michael Grandner, director of the Sleep and Health Research Program at the University of Arizona in Tucson, says researchers now believe the K-complex to be a sign of the brain responding to sensory stimulus and returning to sleep.
Numerous sleep researchers noticed the similarity of the K-complex to other brain waves, namely those that the brain produces during its most restful periods—slow wave sleep. This phase is key to immune function and memory consolidation, and is the phase that tends to become harder to achieve and sustain as humans age.
An EEG of slow wave sleep, a more regular series of high-amplitude waves, looks like this:
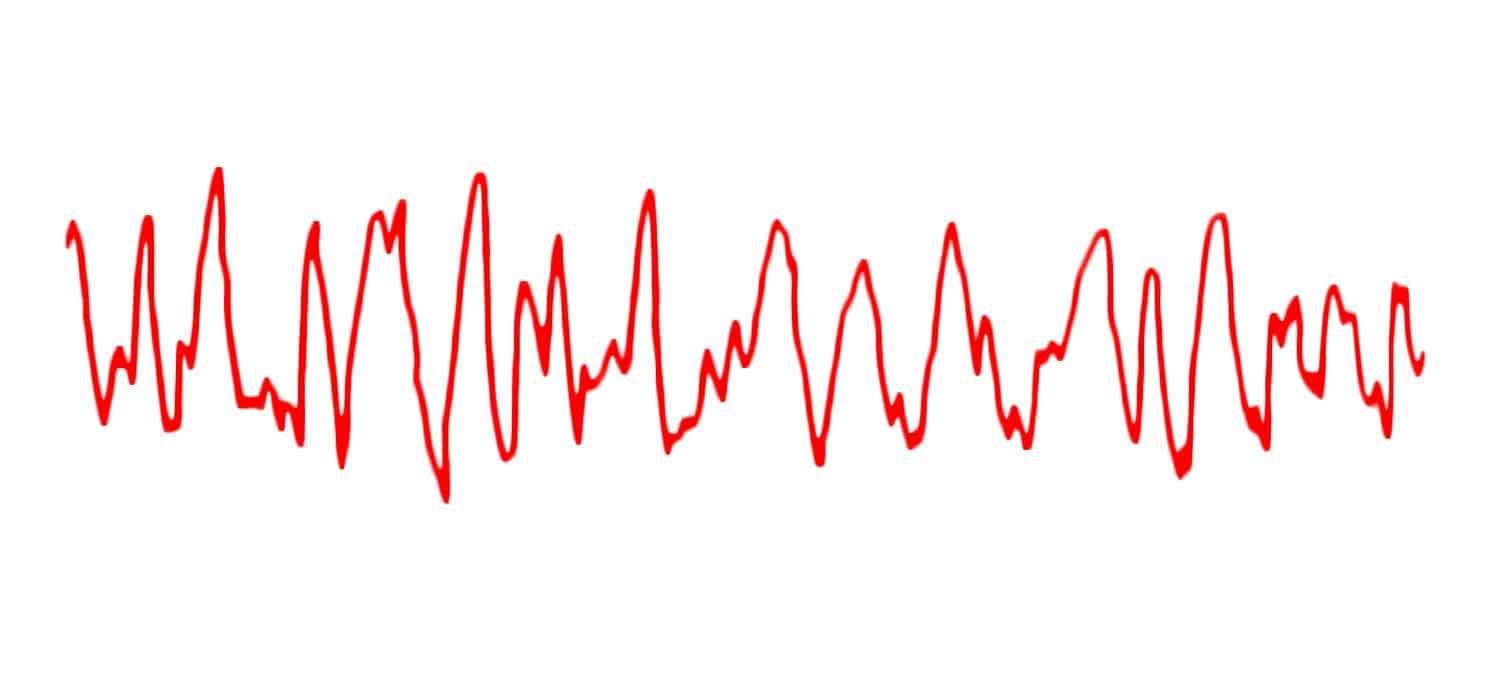
A K-complex looks similar to a single slow wave, a similarity that inspired multiple sleep labs to see if the one could be used to induce the other. By giving the brain a series of nudges—in other words, by triggering K-complexes—could they strengthen the waves into a pattern that mimicked slow wave sleep?
“Acoustic stimulation is exciting, even though it’s very much in the proof-of-concept stage,” says Grandner. “Until now, slow wave sleep has been a lot easier to break than fix, and we can’t reliably stimulate it with drugs.”
The study of acoustic stimulation has spread rapidly over the past few years. Phyllis Zee, director of the Center for Circadian and Sleep Medicine at Northwestern University in Chicago, led a widely cited 2017 clinical study with 13 participants, ages 60 and older. For a stimulus, she used “pink noise,” a relative of the “white noise” of television static, delivered at a level that wouldn’t awaken sleepers. The timing was guided by software, plugged into an EEG.
The software listens for waves that the brain has already initiated and delivers the sound pulses at just the right moment to strengthen those waves, like a parent timing a child’s push on a playground swing. “Timing is very important when it comes to how acoustic stimulation is delivered,” Zee says.
Participants in the Northwestern study who received acoustic stimulation increased their overnight recall of word pairs—a measure of memory—by nearly 27%. A more recent and larger study, from Duke-NUS Medical School in Singapore, used a similar process with younger sleep-restricted participants during a 90-minute nap. They obtained similar findings on an image recognition task.
One pioneer in acoustic stimulation was Jan Born, now director of the Department of Medical Psychology and Behavioral Neurobiology at the University of Tübingen in Germany. In a 2017 Nature Communications paper, Born’s lab showed that acoustic stimulation could reduce the stress hormone cortisol in young volunteers. And while past studies had shown that disrupting slow wave sleep results in diminished growth hormone secretion, acoustic stimulation did not have the reverse effect.
Some companies are already looking to bring consumer products to market. Last year, French startup Rythm began selling headsets that promise to monitor brain waves and deliver sounds that strengthen wearers’ slow wave sleep. Rythm recently published a paper in Frontiers in Human Neuroscience using data from its users’ experiences and a clinical trial, which includes a finding that its effects did not diminish over 10 nights of use. Pierrick Arnal, the scientific director for Rythm, is planning placebo-controlled studies.
Some medical sleep experts, including Grandner, are skeptical about acoustic stimulation’s potential for home use, at least at this point. Still to be answered in clinical studies is whether a series of induced K-complexes are really the same as a slow wave pattern that occurs naturally.
The next steps may involve getting a much closer look at the brain’s internal interactions. Sleep scientists at New York University have been enlisting the help of epilepsy patients undergoing seizure diagnosis, who already have electrodes inserted into their brains. Recording information using those electrodes could help gauge acoustic stimulation to a higher degree to answer additional questions about its impact.
Stay on the frontiers of medicine
Related Stories
- The Brain’s Beat
By studying the mysteries of anesthesia and how it affects the brain, Patrick Purdon may have found a new way to predict Alzheimer’s disease and other neurodegenerative conditions.
- Going Deep
Next-generation MRI machines can look far inside the brain, and map in minute detail where things go wrong.
- How Poor Diet Shapes the Brain
A high-fat, high-sugar diet can cause harm to the hippocampus—and that may lead, perversely, to even worse impulses around unhealthy food.