Published On July 23, 2009
EVEN SEASONED CANCER RESEARCHERS, not usually given to hype, found a case study that appeared in the April 2008 issue of the Journal of Clinical Oncology miraculous. The patient, a 79-year-old woman, had bleeding tumors in her rectum and vagina, metastases of a very rare form of melanoma that affects mucous linings. A few days after she started taking the drug Gleevec, the bleeding stopped, and after four weeks a CT scan showed the tumors melting away. Nine months later, the patient’s condition was stable, and she was still taking her once-a-day dose of Gleevec.
The miracle, of sorts, was that Gleevec, one of the first targeted therapies (so called because they home in on one vulnerable, cancer-promoting mutation in a tumor cell), was never designed to treat melanoma. It was approved in 2001 to target a completely different kind of cancer (chronic myeloid leukemia) in a completely different organ (blood) because it blocks BCR-ABL, one of a class of proteins known as tyrosine kinases, which activate the molecular pathways that relay growth signals, allowing a cancer to flourish. It later turned out that Gleevec (imatinib mesylate) was also effective against c-KIT, another tyrosine kinase and the culprit in most gastrointestinal stromal tumors; the drug has since become the front-line therapy against that rare and previously deadly disease. The discovery that Gleevec can target c-KIT as well as BCR-ABL inspired researchers to try it on other cancers harboring a c-KIT mutation, including this woman’s melanoma.
This progress involving targeted therapies has implications for how cancers are diagnosed and treated and how clinical trials are designed. It adds weight to the idea that, for treatment purposes, tumors often need to be classified not by where in the body they occur but by the genetic mutation that causes them to grow and spread. Although gastrointestinal cancers and melanomas, for example, appear to be quite different, they seem to have much more in common than two kinds of breast cancer.
“The result reported in the Journal of Clinical Oncology sends a crucial message,” says David Fisher, chief of dermatology at Massachusetts General Hospital, who was involved in the melanoma study while at the Dana-Farber Cancer Institute in Boston. “If we know the underlying mutation and we have the right drug to target that mutation, we can treat even widely metastasized cancers for which we’ve had no effective therapy.”
Still, despite the dramatic effects of targeted therapies, they can accomplish only so much; when a drug blocks one pathway a cancer uses, it may take a detour and careen down a cellular bypass, making it resistant to the drug. All too often this means that a patient who experiences a seemingly miraculous recovery may succumb to a recurring cancer. That’s leading to a second generation of therapies designed to overcome tumors’ resistance to first-generation approaches, and drugs of both types now account for almost half of cancer-drug development. Making the best use of these new treatments may require oncologists to proceed much as physicians do when treating infectious diseases: by diagnosing the particular pathogen, in this case a mutation, before prescribing a therapy.
A WIDE ARRAY OF CHANGES CONSPIRE to let cells escape normal checks and balances on growth and behavior. Some mutations silence genes that typically would shut down undisciplined growth. Others cripple the mechanisms that repair DNA damaged during cancer’s rapid, reckless cell division or that, for cells beyond redemption, force them into apoptosis, a programmed suicide. And still others entice malignant cells to metastasize to far-flung organs. Cancer needs all these mutations to develop and flourish, and as it becomes more advanced, it accumulates more and more of them.
Given how many mutations it takes to render cancer cells malicious, it’s remarkable that most targeted therapies succeed by zeroing in on just one of them. This works because many cancers appear to become overdependent on a single cancer-causing gene, called an oncogene, that drives the runaway growth. This dependence gives them an Achilles’ heel, because blocking just this one oncogene with a targeted therapy makes the cancer cell screech to a halt, wither and die. Researchers often speak of this dependence as oncogene addiction, and they refer to the dramatic effect of targeted therapies as oncogenic shock, says Daniel Haber, director of the MGH Cancer Center.
Many addictive oncogenes belong to a large class that produces tyrosine kinases, which Jonathan Fletcher, a pathologist at Brigham and Women’s Hospital in Boston, describes as protein master switches. “They normally stay in the off position until they receive a message that the cell needs to divide,” Fletcher says. “Then they switch on and activate one growth pathway after another, like falling dominoes.”
In cancer, mutations essentially alter the shape of the switch, so it stays in the on position, flashing loud and incessant growth signals to downstream pathways. In targeted therapies, drug molecules latch onto the master switch and turn it off, preventing the kinase from transmitting its signal.
PATIENTS WITH BREAST CANCER WERE THE FIRST to benefit from the notion that a tumor’s molecular characteristics could guide treatment. During the 1980s, clinical research showed that most breast cancer tumors had receptors for estrogen, allowing the hormone to stimulate the cancer’s growth. The drug tamoxifen, which had been recently developed, treated these cancers by blocking the estrogen receptor and depriving the cancer of this growth signal. But tamoxifen wasn’t effective against breast cancers that did not have estrogen receptors, so doctors began dividing breast tumors into these two genetic subgroups before determining whether to prescribe the drug. Then, in 1987, Dennis Slamon, an oncologist at the Jonsson Comprehensive Cancer Center at the University of California, Los Angeles, found another important subgroup. “There was great disparity in how well women did on chemotherapy,” Slamon says. Those who did worst, he discovered, had an excess of HER2, a protein receptor. In normal quantities, HER2 produces the kind of growth signal that all cells need occasionally. But having too much amplifies the signal, turning it malignant.
The discovery of HER2’s role in the very worst cases of breast cancer was bad news indeed, until Slamon followed a hunch. Most therapies target cells that divide at a faster-than-normal rate. That’s a reasonable approach, because no cells divide more quickly than cancer cells. But cells in the skin, hair follicles, white blood cells and intestines also divide frequently, and they, too, are killed, leading to such side effects as hair loss, nausea and a weakened immune system. Slamon’s notion was to develop an antibody that zeroed in on HER2 as a distinguishing genetic feature of the cancer cell, with the hope that it would do a better job of killing the cancer while also causing fewer side effects. That antibody, Herceptin, identifies HER2 and signals the body’s immune system to destroy the cell.
Herceptin (trastuzumab), in conjunction with chemotherapy, improved the cure rate for women with the HER2 amplification by about 40%. On the heels of Herceptin’s success came Gleevec, a tyrosine kinase inhibitor that doesn’t need to be accompanied by chemotherapy and has been remarkably effective against some tumors. Since then there have been additional tyrosine kinase inhibitors (some still in trials) for melanoma and cancers of the lung, kidney, colon, stomach, head and neck, among others.
“We now know that two breast cancers may have nothing in common except the breast because they activate different genetic pathways,” Slamon says. “Today every breast cancer patient has her tumor classified by its genetic subtype.” He thinks that most cancers, if not all, can be broken down into genetic subtypes.
But just as tumors that develop in the breast may have different genotypes, those that arise in remote body parts may have strong genetic connections. The HER2 amplification also occurs in some cancers of the lung, esophagus, salivary glands and ovaries, and Herceptin may work against those cancers too. “This means we don’t always have to start from scratch and develop an inhibitor or antibody for each cancer,” says Jeffrey Settleman, director of the Center for Molecular Therapeutics at the MGH Cancer Center. “We can repurpose existing ones.”
That new treatment paradigm means changing not only clinical practice but also how cancer drugs are tested. To illustrate the challenge of constructing clinical trials to evaluate targeted therapies, Haber of the MGH Cancer Center points to two drugs, Iressa (gefitinib) and Tarceva (erlotinib), that were ineffective as first-line treatments for most forms of lung cancer. Haber thinks the promise of those therapies was squandered by their having been tested too broadly.
Both drugs target a tyrosine kinase called EGFR that, Haber and his colleagues discovered, is mutated in just 10% of non-small-cell lung cancers (NSCLCs) in the United States. As a result, the drugs had little effect on the vast majority of NSCLCs and were relegated to use as third-line treatments, which may extend a patient’s life by mere weeks. But recently in Asia, where EGFR mutations are more common, Iressa was dusted off for a more rigorous trial that compared its benefits with those of chemotherapy in patients with and without the EGFR mutation. As Haber had hoped, patients with the mutation had a 50% lower risk of cancer progression if they took Iressa than if they’d undergone chemotherapy. Those without the mutation did better on chemotherapy and roughly three times worse on Iressa.
“This shows that molecular profiling can help us make a wiser decision about whether to use Iressa or chemo as first-line therapy,” Haber says. And it underscores the need for clinical trials that look beyond broad populations to consider small subsets of patients with particular mutations.
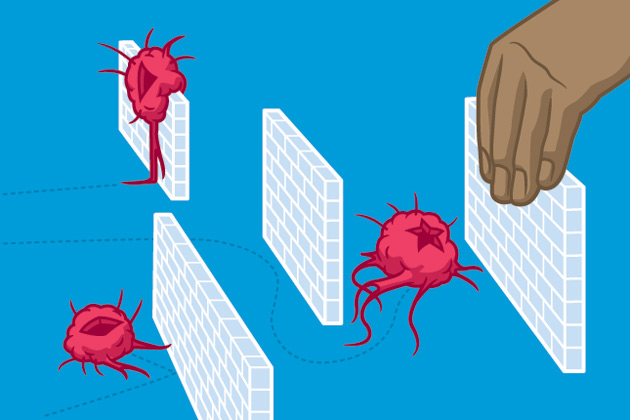
AS PROMISING AS TARGETED THERAPIES ARE, virtually all patients who respond well at first to these drugs eventually relapse, though how soon the cancer returns varies greatly. Leukemia patients on Gleevec may do well for many years, whereas patients with advanced kidney cancer who receive a targeted therapy called Sutent (sunitinib malate) may experience benefits lasting only six months. “Cancer is clever, and it uses more than one pathway,” explains Nancy E. Davidson, a breast cancer researcher at the University of Pittsburgh Cancer Institute. “Block one path, and it will often come back on another.” It may also mutate the original target so that an inhibitor can no longer attach there and block the cancer pathway. Davidson says that although oncogene addiction is an attractive hypothesis, cancer’s enormous complexity sometimes reasserts itself. “My guess is it will be the rare cancer for which we can target a single oncogene,” she says.
According to Haber, it’s possible that just 10% to 20% of cancers have single addictions. But some of these cancers are unusually aggressive or respond poorly to traditional therapies, so for them targeted inhibitors are major breakthroughs.
Moreover, even when targeting a single tyrosine kinase does not shut down a tumor completely, it may be possible for a combination of kinase inhibitors to achieve that goal. In addition, these drugs can be effective not only against the tumor but also in suppressing the body’s reaction to the tumor, which can enhance its growth. For example, Sutent, a tyrosine kinase inhibitor, is also thought to suppress angiogenesis—the formation of tumor-supporting blood vessels—and has proven effective in treating advanced kidney cancer.
“It’s becoming fairly straightforward to identify targets in cancer cells, and it’s not so hard to find drugs to inhibit them,” Fletcher says. “The real challenge is understanding the molecular mechanisms that drive resistance to the drugs and then coming up with treatments that can shut down those mechanisms.” This approach is leading to second-generation drugs that overcome resistance to simpler targeted therapies.
While at UCLA, researcher Charles Sawyers discovered that resistance to Gleevec in chronic myeloid leukemia was caused by mutations in ABL, the tyrosine kinase the drug targets. Gleevec binds to ABL only when its switch is in the off, or closed, position. But when ABL mutates, Gleevec no longer has an effect.
To figure out why, Sawyers and his colleague John Kuriyan of UC Berkeley used X-ray crystallography, which directs light through crystallized molecules in a way that details their 3-D structure, including the nooks and crannies where drugs bind to proteins. They looked at ABL in both its active state, with the switch open, and its inactive state, or off position. “When ABL is open, it looks just like another open tyrosine kinase called SRC, even though they don’t look alike when they’re closed,” says Sawyers, now in the human oncology and pathogenesis program at Memorial Sloan-Kettering Cancer Center in New York City. It turned out that Bristol-Myers Squibb was working on SRC inhibitors, and one of those became Sprycel (dasatinib), a second-generation drug that attaches to both the open and closed ABL.
After an initially strong response to Gleevec, gastrointestinal stromal tumors have also become resistant by acquiring mutations in the c-KIT tyrosine kinase that the drug targets. Two second-generation drugs can now inhibit those mutations. But it may be only a matter of time before the cancers develop resistance to those therapies, and Fletcher is trying several approaches that rely on knocking out the proteins on which c-KIT depends.
One alternative target is a kinase called PI3K, which lies downstream of c-KIT in the growth-signaling cascade. C-KIT passes its command to grow through this protein. In an early clinical trial, Fletcher found that knocking out PI3K with an inhibitor stops the growth signal. “No matter what mutation c-KIT picks up to escape Gleevec,” he says, “it still needs to send its signal through PI3K, so adding this inhibitor to Gleevec is an appealing idea.”
A second approach involves targeting a type of protein known as a chaperone, which keeps c-KIT stable and properly formed. Form is function when it comes to proteins, whose shapes determine what they can latch onto and activate. Without the guiding hand of a chaperone called HSP90, c-KIT can’t function. In this approach too, it won’t matter how c-KIT mutates if its chaperone is missing. To prevent resistance, Fletcher foresees combining such therapies with Gleevec from the start.
DESPITE THE PROPENSITY OF A TARGET to mutate or a cancer to activate alternate pathways, targeted therapies and their offshoots continue to inspire optimism among researchers. “When cancers become resistant to various forms of chemotherapy, we have no idea what the mechanism of resistance is,” Haber explains. “But when cancers develop resistance to a targeted therapy, we can zero in on the targeted pathway and figure out the mechanism through molecular analyses.” Shut down enough of these mechanisms, and you should be able to keep the cancer from coming back, he adds.
For this approach to have widespread success, physicians will need the means to test patients’ tumors to determine the most appropriate treatment—and what to turn to next when a first-line therapy falters. For example, the lung cancer drugs Iressa and Tarceva succumb to resistance, in some cases, because of new mutations in the EGFR oncogene. But resistance may also begin when the tumor switches its dependence to MET, another tyrosine kinase. Although second-generation drugs are being created to handle both problems, doctors won’t be able to prescribe the right one without testing a patient’s tumor cells to find out which resistance mechanism is involved.
Some tests to make those determinations are already commercially available, but others await development, and demand from clinicians could help speed the task along. Earlier this year, the American Society of Clinical Oncology recommended that before prescribing Erbitux (cetuximab) for colon cancer patients, doctors should screen patients’ tumors for a KRAS mutation (another tyrosine kinase) that negates the drug’s benefits. “Overnight we started getting calls from oncologists wanting to test their patients,” says John Iafrate, a pathologist who runs the Clinical Molecular Diagnostics Laboratory at the MGH.
Many researchers think that treating cancer will come to follow an infectious disease paradigm. Before prescribing a therapy, doctors will send a tumor sample to the pathology lab to identify the oncogenic agent, and that information will guide therapeutic choices. And like AIDS, many cancers will require cocktails instead of single-agent drugs.
“But we can’t take the same approach we took with chemotherapy combinations, in which we just mixed and matched them and tested them in thousands of patients in hopes of a better outcome,” says Slamon of UCLA. “We need to do things the right way with targeted therapies”—selecting patients for smaller trials according to whether they have the genetic anomalies that targeted drugs are designed to attack; using the resulting therapies based on tumor genotypes; and continuing to find ingenious ways to overcome cancer’s resistance to the latest generation of drugs.
Dossier
“Oncogene Addiction,” by I. Bernard Weinstein and Andrew Joe, Cancer Research, May 1, 2008. This brief article explains how some tumors may develop an overdependence on certain cancer-promoting genes and why deactivating those pathways with targeted therapies can cause tumors to rapidly regress—at least temporarily.
“Herceptin,” by H. Michael Shepard, Pei Jin, Dennis J. Slamon, Z. Pirot and Daniel C. Maneval, Handbook of Experimental Pharmacology (Springer-Verlag, 2008). A summary of the pivotal events in the development of the first targeted therapy, Herceptin, for the approximately 25% of breast cancer patients whose tumors are vulnerable to the drug.
“Epidermal Growth Factor Receptor Mutations in Lung Cancer,” by Sreenath V. Sharma, Daphne W. Bell, Jeffrey Settleman and Daniel A. Haber,Nature Reviews Cancer, March 2007.This article summarizes evidence that a particular mutation in lung tumors can predict whether a patient will respond well to targeted therapies that inhibit it and hints that such drugs were tested too widely.
Stay on the frontiers of medicine