Published On November 20, 2021
Peter Vieira was 39 when he was diagnosed with a malignant brain tumor, a stage 2 astrocytoma the size of a golf ball lodged in the temporal lobe of his brain. Although the cancer was growing slowly, its location meant treatment would be perilous. The first step was to excise the tumor, but because it was in the brain, Vieira’s surgeons couldn’t remove an additional swath of healthy tissue to make sure they had all of the cancer cells. Radiation therapy could kill the straggler cells, but with conventional photon radiotherapy, which uses high-powered x-rays, some radiation would pass through the cancer, bringing not only an immediate risk of damage to the brain or pituitary gland but also elevating the risk of other cancers years later.
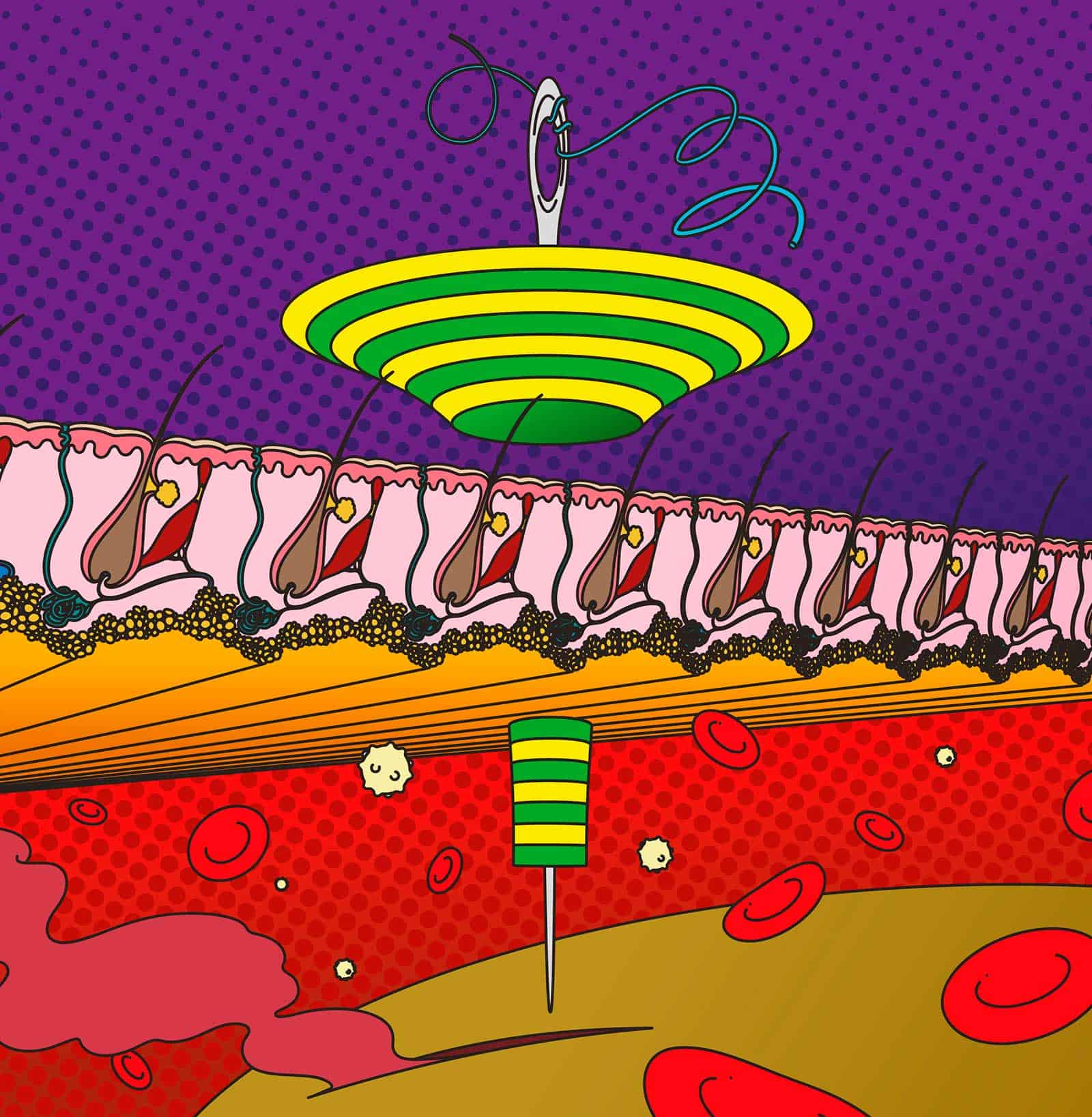
Vieira’s doctors suggested an alternative. They invited him to join a clinical trial assessing proton therapy, a different kind of radiation treatment. That technology, in use for decades, relies on proton particles split from hydrogen atoms and then spun around an accelerator called a cyclotron, extracted and guided by magnetic fields to the tumor. A key advantage is that the energy of the protons can be precisely calibrated, which means that technicians can control how far they penetrate into the body. Proton therapy can hit a tumor with a heavy dose of DNA-altering radiation that is released there, like a tiny precision strike, going no farther. Vieira agreed to try it.
For many cancers, this more targeted approach to treatment should be ideal. “A technique that can achieve a higher dose of radiation to the tumor while delivering equal or less radiation to normal tissues—that is by definition a superior treatment,” says Helen Shih, medical director of the Massachusetts General Hospital Proton Therapy Centers, where Vieira was treated. And since the tool’s origins at the dawn of the Atomic Age, increasingly sophisticated forms of proton therapy have been developed and deployed to treat an ever wider range of malignancies. It is now routinely recommended for most pediatric cancers and adult head and neck cancers—applications that speak to its specific advantage, namely a precision that can help avoid debilitating side effects and reduce the risk of later cancers. That precision also makes it a sought-after tool for prostate cancer, where incontinence and impotence are often a risk, and others have looked at its usefulness in breast and lung cancer treatment.
To meet increasing demand, hospital centers that offer the proton therapy have sprung up around the world. As of last October, they numbered 40 facilities in the United States and more than 100 globally. MGH, a pioneer in proton therapy and the first to have a treatment center, opened a second center in 2020, and other big names in cancer treatment—Memorial Sloan Kettering, MD Anderson, Johns Hopkins, Mayo Clinic—now also offer it. Japan has 24 centers and a handful of others exist in Germany and the United Kingdom, while Denmark and Norway have recently joined the movement.
The future of proton therapy, however, depends heavily on the technology finding its therapeutic groove. The centers are very expensive to build and operate—the cost of treatment is often several times that of conventional radiotherapy, and insurance companies have long been reluctant to reimburse patients, denying as many as two-thirds of requests for coverage. In a 2016 editorial, Anthony Zietman, currently the interim chief of radiation oncology at MGH, lamented that proton therapy was still trying to shake off a reputation for being “exotic, expensive and irrelevant.” The field has made advances since then, but still lacks key clinical trial data to support many of its applications.
Major efforts now in progress, however, appear to be on the cusp of changing that. Trials like one that helped Vieira with his brain tumor aim to determine how, and how extensively, proton therapy works, and that data will be the key to determining its place in cancer treatment in the coming decade.
Proton therapy can trace its origin to 1930 and the invention of the cyclotron. That massive machine, created by Ernest Lawrence at the University of California, Berkeley, was designed to break apart the nucleus of hydrogen atoms into their subatomic parts—positively charged protons and uncharged neutrons—and then accelerate them around a track using an electromagnetic field. Its original purpose was to probe the secrets of matter. But in 1943, a cyclotron at Harvard University was sold to the U.S. government for $1, dismantled and sent to Los Alamos, New Mexico. There it was used in the Manhattan Project, the secret effort to create an atomic bomb.
As part of that agreement, the government promised either to return the cyclotron when it was no longer needed or to pay for the construction of a new one. And after the war, physicist Robert R. Wilson, a veteran of the Manhattan Project, came up with an idea that would put that new Harvard cyclotron to peaceful use. Eager to atone for his involvement in building the bomb, Wilson, then an associate professor of physics at Harvard, published an article, “Radiological Use of Fast Protons,” in the November 1946 issue of Radiology. Wilson suggested that the properties of protons “make it possible to irradiate intensely a strictly localized region within the body, with but little skin dose.”
protons could be guided to hit a tumor and nothing else.
In the article, Wilson pointed out the unusual behavior of protons. The particles tend to travel through materials in a straight line until they come to a stop and release all of their energy. That large jolt is called “The Bragg Peak,” and Wilson surmised that it could be a boon to cancer therapy. Unlike high-powered X-rays, which have a tendency to scatter and irradiate adjacent tissue, protons could be guided to deliver DNA-altering radiation to a tumor and hit nothing else.
The cyclotrons in existence at the time, Wilson noted, weren’t powerful enough to create a beam of protons that could reach a human tumor. But newer machines, then planned or under construction, would have a far greater range. “It is clear,” he wrote, “that such protons can penetrate to any part of the body.”
After Wilson’s article was published, physicists and physicians began to explore how this new kind of treatment, which seemed at least theoretically feasible, might be developed. The first patients to receive proton therapy were treated at the Berkeley Radiation Laboratory in Berkeley, California, in 1954, and in 1957, at a facility in Uppsala, Sweden.
But most of proton therapy’s early history involved close collaborations between the Harvard Cyclotron Laboratory (HCL) in Cambridge and physicians at MGH. In 1971, Herman Suit, head of radiation oncology at the hospital, recruited a British physicist, Michael Goitein, who threw himself into nascent efforts to explore the possibilities. In spring 1972, Goitein organized a one-day symposium that brought together MGH physicians and nuclear physicists from Harvard, MIT and the Princeton Particle Accelerator Laboratory. Out of that forum came not only a consensus that proton technology had therapeutic possibilities, but also a plan to explore them on-site.
By 1973, the project was ready for its first patient, a four-year-old boy with a pelvic tumor. Because the HCL facility lacked a gantry—the movable arm that in modern systems can pivot around a patient—patients had to be positioned in whatever way made their tumor most accessible to the giant machinery. Some sat or stood, and they had to remain as still as possible so that the proton beams could reach their target.
In those early days, physicists, doctors and patients had to share space with graduate students from the physics department who took over the HCL in the afternoon. Then, as now, extensive imaging had to precede each treatment, to determine the exact size and location of the tumor and create a plan for positioning the proton beam. That preparation was done at MGH, with patients then ferried, often by taxi, on the 20-minute ride to the lab in Cambridge.
Ultimately, some 4,500 MGH patients were treated at the HCL. By the early 1980s, however, two things were clear: Proton therapy could be an extremely effective way to treat many cancers, and the hospital needed a proton therapy treatment center on its own campus. After a decade of planning and fundraising, construction began on a cyclotron, two gantries and three treatment bays. Finally, in 2001, MGH opened the Francis H. Burr Proton Therapy Center, the first hospital facility created to provide proton therapy.
Today, treating one person’s cancer with proton therapy may cost from $30,000 to $120,000, compared with just $8,000 to $15,000 for a course of conventional radiation therapy. That much higher price tag, one of the main concerns for the future of proton therapy, factors in the much higher cost of building and maintaining these facilities, the complicated engineering that goes into running the equipment and the expertise needed to tailor treatments.
In many cases, however, the side effects of the alternative—conventional radiation therapy—can also be expensive, both in human suffering and medical costs. MGH’s Helen Shih notes that in head and neck cancers, for example, patients who undergo traditional radiation therapy may suffer a range of ills: permanent dry mouth that prevents swallowing and causes choking, dental and spinal deformities, damage to the thyroid gland, chronic pain and cognitive dysfunction. Symptoms can be so severe that they result in the need for a feeding tube.
For head and neck cancers, insurance companies do often approve proton therapy. But for many other conditions—especially those such as breast and prostate cancers that affect large numbers of patients—they have shown reluctance. Their decisions are buoyed by a 2014 report for the Institute for Clinical and Economic Review, a Boston nonprofit that evaluates the cost-effectiveness of medical care, which stated that the cost of proton therapy was justified for only a few select types of cancer, including pediatric and brain and spinal tumors.
This was the first clear victory for proton therapy in a head-to-head contest.
Harald Paganetti, director of physics research in the Department of Radiation Oncology at MGH, notes that proton therapy should be a better choice in most cases when judging by the dose distribution alone. “If you simply look at it from a physics perspective, protons and photons give the same amount of radiation to the tumor, but the dose that goes to the surrounding tissues with proton therapy is much smaller, on the order of two to five.” That underscores why proton therapy is so beneficial for children, whose young tissues are more susceptible to the harmful effects of radiation. Evidence shows that children who receive proton therapy have a much lower incidence of cognitive decline, for example, than those who got conventional therapy. “There is clearly an advantage for pediatric cases,” he says. “But for others, the benefits are less clear.”
Evidence of the comparative merits of the two kinds of radiation is only now beginning to be amassed, and it promises to show just where proton therapy can do the greatest good—and where it might not be needed. The first randomized trial to evaluate proton therapy in lung cancer, for example, was published in the Journal of Clinical Oncology in January 2018. Proton beam therapy and traditional radiotherapy, it showed, were equally effective in treating the tumor and showed no difference in a common side effect that results in severe inflammation in the lung that sometimes requires hospitalization.
Brian Baumann, a radiation oncologist at Washington University School of Medicine in St. Louis and the University of Pennsylvania, wonders whether the choice of radiation-induced lung injury as a primary endpoint might have limited the 2018 study’s ability to detect a potential benefit for proton therapy in reducing overall side effects. “I suspect that if the study had used the overall rate of severe toxicity—which includes a wide range of side effects—as its endpoint, it may have reported more of a benefit for proton therapy,” Baumann says.
In 2019, Baumann was the lead investigator for the first large-scale review comparing proton beam therapy and conventional therapy across multiple cancer types for patients treated with concurrent radiation and chemotherapy. The study, published in JAMA Oncology, analyzed data from about 1,500 adult patients with 11 kinds of cancer. Patients receiving conventional treatment were more than twice as likely to experience a severe toxicity that leads to hospitalization or an emergency room visit, they found. In addition, the patients’ abilities to perform routine activities were half as likely to decline for the proton therapy group. The study did not include prostate cancer patients or breast cancer patients who were rarely treated with concurrent chemotherapy and radiation.
And in 2020, a study published in the Journal of Clinical Oncology showed positive results for esophageal cancer patients. Patients were randomized to traditional or proton radiotherapy, and those who received proton therapy had significantly fewer adverse events and an improved survival rate. According to an accompanying editorial, this was the first clear victory for proton therapy in a head-to-head contest with conventional radiation.

Further evidence should come in the next few years from several large randomized clinical trials. The biggest of those is the COMPARRE (COMparative Study of Outcomes with Proton and Photon Radiation in Prostate CancER), begun in 2018 and led by researchers at the University of Florida, which plans to recruit 1,500 patients for each arm of the study. And the RADCOMP trial, launched in 2015 and led by researchers at MGH, the University of Pennsylvania and Memorial Sloan Kettering Cancer Center, is recruiting patients to see whether proton therapy can reduce cardiovascular events—heart attacks, arrhythmias and valve disorders—related to radiation treatment in breast cancer patients. According to Shannon MacDonald, an MGH oncologist and lead investigator of the trial, the proliferation of proton therapy centers will make it easier to recruit patients and collect needed data.
MGH’s Anthony Zietman agrees. “We’ve reached a critical mass with the number of proton centers in America,” he says. “Now we can actually do multicenter trials and get them done quite quickly to answer questions about where the benefit lies and where it doesn’t.”
Even as research ramps up, the technology of proton therapy is changing rapidly, as engineers explore ways to bring down the cost and make the systems easier to install. When the first MGH proton center was built 20 years ago, the massive component parts came first, and an entirely new building had to be designed to fit around them. New, smaller cyclotrons may be able to fit in existing spaces.
Other advances are improving accuracy. Pencil beam scanning, for example, introduced during the past decade, allows the proton beam to penetrate the tumor more precisely, layer by layer. Increasingly, real-time imaging systems are built in, so that protons can be more accurately applied even to moving tumors, such as those in the lungs. “That lets us control the beam to improve accuracy even more,” says Aswin Hoffmann, a medical physicist at OncoRay in Dresden, Germany.
These efforts to reduce costs and increase performance, alongside results from the major trials now underway, could go a long way toward answering lingering questions. “At the end of the day, if protons could be as affordable as any other kind of radiation, and as easy to deliver, there would be no discussion,” says Helen Shih. “We would all be using protons.”
“The two sides of the equation are research and cost,” adds Zietman. “On one side, you can target the patients who benefit most from this treatment, while on the other side, you work to decrease the costs. And that way you increase value all around.”
Dossier
“Three Ways to Make Proton Beam Therapy More Affordable,” by Thomas Bortfeld and Jay Loeffler, Nature, September 2017. The paper explores advancements in engineering, physics and health care policy that could bring down the cost of proton beam therapy. They include shrinking the size of accelerators, making the tool more accurate and broadening coverage.
“Can Proton Therapy Be Considered a Standard of Care in Oncology? Lessons from the United States,” by Anthony Zietman, British Journal of Cancer, March 2020. This brief summary of the evolution of proton beam therapy looks at present and future challenges, as well as the role that the United Kingdom might play in conducting research.
Stay on the frontiers of medicine
