Published On January 15, 2010
IN MEDICAL SCHOOL IN NAPLES, IN THE LATE 1970S, Alessio Fasano learned a thing or two about human intestines. More than twenty feet long, with an interior surface a bit bigger than a tennis court (about 3,000 square feet if you include the shaggy, finger-shaped villi that grab nutrients from digested food and drink), the intestines are lined with epithelial cells that were thought to be sealed permanently by groutlike junctions. Tiny nutrients are absorbed through the cells, but the “grout” was credited with creating an impermeable barrier preventing larger, harmful material from entering the gut. Then, in the late 1980s, when Fasano was working on a cholera vaccine, he began to wonder how large molecules, such as the cholera toxin, got past the intestinal wall and into the bloodstream, and learned that the space between cells was not sealed after all. His suspicions were confirmed in 1988, when a Japanese research group discovered that the “tight” junctions are actually perfectly fitted doors that open and close under special circumstances.
Fasano, who now directs the Mucosal Biology Research Center and the Center for Celiac Research at the University of Maryland School of Medicine, hypothesized that the cholera bacterium, Vibrio cholerae, had evolved a key to that door, and he proved the notion in 1991. Using Latin for tight junction, the key was named “zonula occludens toxin,” or Zot. “Vibrio uses Zot to make the intestine permeable,” he says, “and intestinal permeability allows access to the things that can harm us.”
In 2000, Fasano discovered that the body produces its own key, a molecule he called zonulin. Scientists are still trying to determine zonulin’s normal function, but they do know that bacteria and inflammatory molecules can stimulate its production to make the intestines “leak.” It turns out that certain undigested portions of gluten, the storage protein of wheat, barley and rye, may have the same effect.
This accumulating understanding of how, when and under what circumstances the intestines can be breached ultimately led Fasano to an innovative and somewhat controversial theory about autoimmunity—in which the body mistakenly turns on itself—and about one of its clearest examples, celiac disease, in which the autoimmune response is triggered by gluten. He had become interested in celiac disease after searching the scientific literature for references to intestinal permeability and finding that it occurs in many autoimmune diseases—from type 1 diabetes and multiple sclerosis to rheumatoid arthritis and inflammatory bowel diseases, including celiac. That people with autoimmune diseases also have elevated levels of zonulin in their gut could partially explain this leakiness, Fasano reasoned.
In autoimmunity the human immune system, rather than protecting the body from dangerous microbes, goes on the attack against the body’s own cells. Part of the cause is genetic, but to develop an autoimmune disorder, people also need to be exposed to an environmental trigger, such as bacteria or food. Somehow the interaction of genes and trigger generates autoantibodies, which recruit the immune system to destroy a particular type of cell—the insulin-producing pancreatic beta cells in diabetes, for example, or neurons in multiple sclerosis or intestinal epithelial cells in celiac disease.
For an autoimmune disease to take hold requires all three legs of the triad: predisposing genes, the appropriate environmental trigger and the autoantibodies that subvert the immune system’s normal, protective function. For most autoimmune diseases, the triggers and even the genes remain unknown, but in the case of celiac disease, all three legs of the triad have been identified. Scientists have found some of the genes and the autoantibodies, and they know that gluten in the diet triggers symptoms. Celiac disease is also the only autoimmune disorder for which there’s a cure—removing the trigger. Stop eating gluten, and the autoimmune response will end, returning the intestines to normal.
It would be ideal, of course, if all autoimmune disorders were as easily curable as celiac disease, which afflicts an estimated one in 133 people. But while researchers attempt to find other genes, triggers and autoantibodies associated with other diseases, Fasano wonders whether there might be a simpler approach. What if some of these diseases also depend on intestinal permeability for getting the environmental trigger into the body? If that was the case, a drug that could prevent the tight junction door from opening might reverse the progress of these diseases, even if their triggers remain unknown.
“It’s a nice hypothesis,” says Detlef Schuppan, a gastroenterologist at Beth Israel Deaconess Medical Center in Boston. Yet despite encouraging results from trials of a drug that attempts to close off the tight junctions in the intestines, the hypothesis remains unproved. Still, that idea, along with other strategies for removing one or another leg of the triad, is being put to the test. “With celiac disease,” says Joseph A. Murray, a gastroenterology researcher at the Mayo Clinic in Rochester, Minn., “we now have a window into how autoimmunity occurs”—and a way to test new therapeutic strategies.
THE HUMAN INTESTINE, THE BODY’S LARGEST INTERFACE with a world full of hazardous microorganisms and toxins, is the most common avenue for infectious organisms invading the body. To counter such attacks, the lamina propria, a moist mucosal layer beneath the epithelial lining, teems with immune cells. But the intestine also hosts beneficial microorganisms that aid digestion, as well as essential particles from our diet. So the immune system needs an elaborate mechanism to distinguish between what is benign and what is dangerous and should be attacked. “The immune system in the gut is meant to be tolerant,” says Murray. “It’s mostly welcoming, though in a cautious way. But if it encounters a danger signal, it puts up its guard, and everything that comes in at that time is considered suspect.”
Macrophages and dendritic cells survey the intestinal periphery, asking at each encounter: “Are you part of me, or are you not? And if you’re not, are you friend or foe?” They find the answers posted on a cell’s surface, attached to histocompatibility leukocyte antigen (HLA) molecules. These molecules display to the rest of the immune system bits of a cell’s proteins that serve as name tags, or antigens, that can generate an “anti” response, such as inflammation or antibody production.
The immune system learns to recognize the antigens from the body’s own cells as “self” and also to tolerate the many “nonself” tags on beneficial intestinal microbes and food particles. But in some people, the immune cells misread the antigens attached to HLA, mistaking, say, pollen for a cold virus or gluten for a toxin. Then they send out a faulty danger signal that makes their body’s own cells look suspicious, summoning other immune cells to attack the body’s tissue.
That loss of tolerance happens in celiac disease, but only in people whose genes produce a specific subtype of HLA molecule. Some 85% to 95% of celiac patients have HLA DQ2; the rest have HLA DQ8. But even among those who have one or both subtypes, only some get sick—and only if they eat gluten.
Suppose someone eats a piece of toast. Digestive enzymes home in on particular sequences along the gluten protein’s amino acid chain and cleave them so that the gut can absorb the component amino acids and send those nutrients to the bloodstream. But gluten is such a relative newcomer to the digestive system—humans began cultivating grain just 10,000 years ago—that the body hasn’t evolved enzymes that can break apart an unusual cluster of glutamine and proline amino acids. Some of the undigested protein fragments, or peptides, are excreted, but others may linger in the small intestine. As Fasano showed, gluten peptides stimulate the release of zonulin, the protein that opens the doors in the intestine’s tight junctions and allows gluten to squeeze through into the immune-cell-rich mucosal underlayer. And some gluten is absorbed directly into the epithelial cells, which release the peptides into the same underlayer, where the immune cells await.
NO ONE KNOWS EXACTLY WHAT HAPPENS DURING THE FIRST ENCOUNTER between gluten peptides and the immune system, but scientists think that in most people, macrophages, B cells and dendritic cells gobble up the intruders, completing what the digestive enzymes couldn’t do on their own. In someone with celiac disease, however, inflammation and possibly gluten itself cause intestinal cells to secrete an enzyme called tissue transglutaminase 2 (TTG). In 1997, Schuppan and his team discovered that the combination of TTG and gluten peptides induces certain B cells to produce antibodies to the gluten peptides and TTG—the autoantibody in celiac’s immune triad. Finding autoantibodies to TTG in the blood has become a reliable way to diagnose active celiac disease.
The TTG enzyme, it turns out, is crucial to celiac’s pathology because it reacts with gluten, transforming it into a “super antigen” that has a magnified effect on other immune cells. Even that result wouldn’t ordinarily be a problem, says Murray: “Our gut is used to seeing all kinds of strange things.” But this excessively immunogenic form of gluten fits perfectly into the two forms of HLA molecules (DQ2 and DQ8) that predispose people to celiac disease. It doesn’t fit any other variety of HLA.
Only when the gluten antigen is displayed on these two HLA molecules can it activate T cells (Th1 and Th2), which then alert other white blood cells belonging to something called the adaptive immune system, which responds to what it considers specific threats. “This sets off a cyclone of activities that feeds on itself and creates a lot of damage,” says Murray.
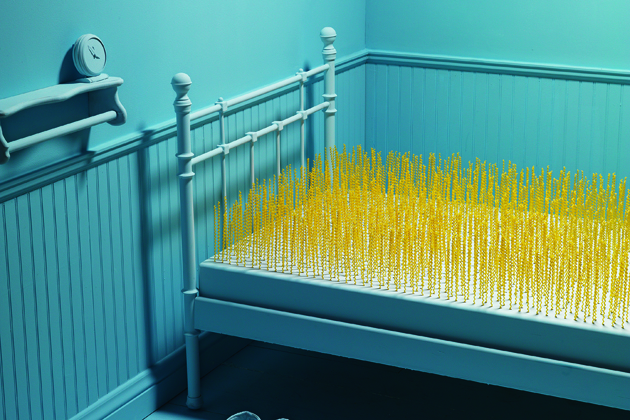
Swirling within that maelstrom are cytokines that induce inflammation (which makes the lining of the gut even more porous), destroy intestinal cells, remodel intestinal connective tissue and, in advanced stages, decapitate the intestinal villi. Without the villi, even someone who eats a healthy diet won’t be able to absorb nutrients effectively and could suffer nutrient deficiencies and malnourishment.
This intestinal turmoil can cause symptoms beyond celiac’s typical diarrhea, bloating and gas, including anemia, bone loss, neurological problems, inflammatory arthritis, hepatitis and even intestinal malignancies and lymphomas. With the ability to screen people for the disease and a growing understanding of celiac disease’s range of symptoms has come the realization that it is not nearly as rare in the United States as researchers once believed. Approximately 1% of the U.S. population is now thought to have celiac disease, about the same prevalence as in Europe and elsewhere. It is about twice as common as rheumatoid arthritis and much more prevalent than multiple sclerosis. Celiac patients also have an unusually high incidence of other autoimmune diseases, probably because those disorders involve some of the same genes. Still, while celiac disease can’t happen without HLA DQ2 or DQ8, just 3% to 5% of people who carry the genes for those molecules go on to develop the disease.
THE AMAZING THING ABOUT CELIAC DISEASE IS that except in rare refractory cases, without gluten, TTG no longer oozes out of intestinal cells, the autoantibody disappears from the bloodstream, the epithelial cells close up their tight junctions and rebuild their nutrient-absorbing villi, and symptoms fade away. This has prompted Fasano to suggest that “if we could stop zonulin from opening the door to the intestine, maybe we could stop celiac’s immune response even when gluten is present.”
Alba Therapeutics, a company Fasano co-founded in 2004 to develop a zonulin inhibitor, is now testing such a drug, called larazotide, in a Phase II clinical trial. (Fasano has left the company but still serves on its scientific advisory board and owns stock options.) “The implication is that if it works in celiac disease, maybe it would work in other autoimmune diseases that also have intestinal permeability,” he says.
In fact, Fasano first used larazotide in preclinical studies of type 1 diabetes in rats. His team reported that the intestines of rats that would later develop diabetes started to leak within five to six weeks of weaning. In addition, the rats had increased levels of zonulin. Then, two weeks before the onset of diabetes, the animals developed antibodies to islets that contain insulin-producing beta cells, whose loss causes the disease. But giving rats the zonulin inhibitor limited the production of those antibodies, thereby reducing the incidence of diabetes by 70%.
Alba Therapeutics subsequently received approval to test larazotide in people with celiac disease, and the company reported preliminary results of its human trial at a conference in April. Patients taking the inhibitor who ate small amounts of gluten had fewer celiac symptoms and lower levels of autoantibodies than those on a placebo who also got gluten. “This is the first time a drug has blocked the autoimmune process by blocking a specific mechanism,” Fasano says. (Past efforts had always involved suppressing the body’s overall immune response or using a general anti-inflammatory.)
But Schuppan of Boston’s Beth Israel Deaconess Medical Center notes that patients on the zonulin inhibitor still showed some intestinal permeability, based on an established measure of sugar absorption. What’s more, he adds, “just closing off the tight junctions is not a magic bullet,” because some gluten is also absorbed into the epithelial cells and thence into the lamina propria.
Still, even though the trial didn’t really prove its primary objective—that larazotide closes up the intestines’ tight junctions—the drug did seem to protect patients from the ill effects of gluten. “So it looks like the drug works, but maybe in a different way than hypothesized,” says Peter Green, director of the Celiac Disease Center at Columbia University College of Physicians and Surgeons in New York City.
Another possibility is that larazotide really does affect the tight junctions but that the clinical test used to measure intestinal permeability, which looks at sugar absorption, is too crude to detect the drug’s impact, suggests Daniel Leffler, director of clinical research for the Celiac Center at Beth Israel Deaconess Medical Center, who was an investigator in the larazotide trial. “We all believe that various things can affect leakiness,” he says, “but a lot of us don’t believe a sugar-based test is specific enough to measure that effect.”
SCHUPPAN SUSPECTS THAT THE IDEAL TREATMENT WOULD INVOLVE vaccines and related immunotherapies that work the way allergy shots do for hay fever victims: by introducing a series of tiny doses of an antigen that teach the immune system to tolerate that antigen. “To do that, you need to know exactly which parts of gluten are toxic,” says Robert Anderson, an investigator at the Walter and Eliza Hall Institute of Medical Research in Parkville, Australia. “Then you can target the parts of the immune reaction that cause the disease.”
Anderson thinks he has identified those parts—three specific peptides—and the vaccine he has developed, now in early clinical trials, focuses on the role of the DQ2 version of the HLA molecule. When these immunogenic gluten peptides enter the body by subcutaneous injection rather than through the gut as they normally do, the immune system could learn to tolerate them. In theory the antigen-presenting cells will still display the peptides on the HLA DQ2 molecule, but instead of causing activation, the T cells will become “regulatory” and not trigger an inflammatory cascade. Anderson believes the same principle should apply to other autoimmune diseases in which antigens presented on HLA molecules also activate a T cell response. “Diseases like type 1 diabetes, multiple sclerosis, rheumatoid arthritis and autoimmune thyroid disease use the same T cells, but the T cells choose to react differently, so they affect different tissues,” he says. “Celiac disease has the advantage of being the first human autoimmune disease for which the critical T-cell-activating peptides have been discovered.”
The beauty of inducing tolerance is that it targets only the parts of the immune system that cause the disease, rather than affecting the whole system the way many current immunotherapy drugs do, which leave people vulnerable to infections and other serious complications. Similarly, larazotide, despite uncertainty about how it works, also has a good safety record.
That’s what’s so exciting about knowing so much about the pathology of a disease, as researchers do with celiac disease. As researchers learn how to prevent or treat autoimmunity in celiac disease, they may be able to apply those lessons and to devise better therapies for less well understood autoimmune diseases that are much less easily controlled.
Dossier
“Celiac Disease and Autoimmunity in the Gut and Elsewhere,” by Susan H. Barton and Joseph A. Murray,Gastroenterology Clinics of North America, June 2008.These experts discuss the theory that environmental triggers can interact with the immune system in the gut, leading to the loss of tolerance and autoimmune diseases.
“Review: New and Developing Therapies for Celiac Disease,” by Christina A. Tennyson, Suzanne K. Lewis and Peter H.R. Green,Therapeutic Advances in Gastroenterology, Sept. 1, 2009. This article makes the case for new therapies for celiac disease (because a gluten-free diet is so difficult to maintain) and describes the most promising approaches in development.
“Tight Junctions, Intestinal Permeability, and Autoimmunity: Celiac Disease and Type 1 Diabetes Paradigms,” by Jeroen Visser, Jan Rozing, Anna Sapone, Karen Lammers and Alessio Fasano, Annals of the New York Academy of Sciences, May 2009.In this review, the authors present the controversial hypothesis that intestinal permeability underlies not just celiac disease but other autoimmune conditions as well, including type 1 diabetes.
Stay on the frontiers of medicine
Related Stories
- Gut Feelings
The mysteries of celiac disease prove to be more intricate than expected.
- Is There Still Room for Gluten?
In this video, MGH researcher Alessio Fasano distills fact from fiction in the gluten wars.