Published On September 22, 2005
KNOWING IT WAS A GAME DIDN’T make Ning Tang, a third-year Harvard Medical School student, any less tense. Her patient seemed to be suffering a heart attack; he was having trouble breathing and complained of severe chest pain radiating to his arm. But his plummeting blood pressure complicated the diagnosis. After an EKG, Tang surmised that the problem might be with the right side, rather than the left, of the man’s heart, and that damage to either side could be responsible for the drop in blood pressure.
If Tang administered dopamine, making the heart pump harder and raising the blood pressure, the added stress could jeopardize an already compromised heart. But a second option—administering fluids—would work only if the right-side diagnosis was correct; for a left-side problem, too much fluid might be a death sentence. “I found myself thinking, I’m taking too long to make these decisions,” Tang recalls. With time running out, she called for fluids, then sighed in relief as the patient’s blood pressure began to rise.
Tang’s patient, of course, was a computer-automated mannequin. Yet even months later, every detail of the experience remains etched in her memory. “To be put into that kind of situation, you remember what happened, why it happened and why it could happen again,” she says. “You never want to lose a patient, whether it’s a game or not.”
That’s the thing about medical simulators: They make doctors sweat, and they make them learn. Willingly suspending disbelief, students, residents and even experienced physicians thrust themselves into unfamiliar or uncomfortable clinical situations. They snake catheters through lifelike webs of veins and arteries, treat gaping chest wounds and struggle to revive anesthetized patients who have gone into cardiac arrest. Working as part of a team in the emergency room or surgical suite, they deal with medicine’s often rigid hierarchies. And they make mistakes—some negligible, some fatal. The lessons learned may ultimately save some of the estimated 195,000 patients a year in the U.S. who die because of medical errors. Advocates of simulators believe their widespread adoption could greatly improve those numbers.

SOME OF THE EARLIEST SIMULATORS, still commonly used in medical schools and hospital training programs, are by far the most lifelike. They walk, talk, breathe and moan. But these living, breathing actors, trained to sharpen physicians’ diagnostic acumen by aping the symptoms of various diseases, can’t raise or lower blood pressure on command, fill chest cavities with blood or put themselves under a surgeon’s knife. They aren’t able to take an overdose of medication to see how a young resident will respond, open their arteries to receive catheters or have their hearts stopped and restarted.
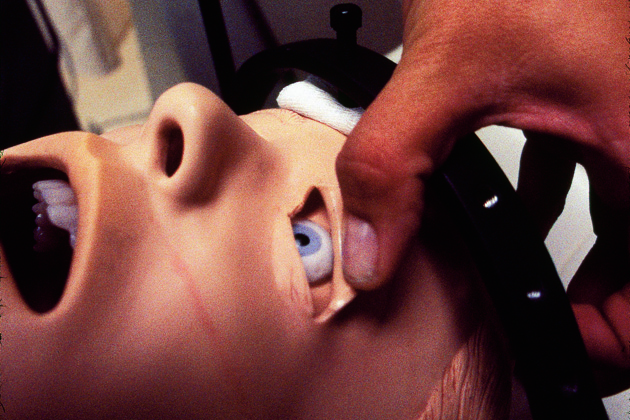
Those tasks are left to mechanical simulators, and after some 40 years of development, today’s most sophisticated models are remarkably adept. Their crude forebears began to appear during the 1960s, creatures of early computer technology. Sim One, designed by engineer Stephen Abrahamson and physician Judson Denson at the University of Southern California, could blink its eyes, open and close its mouth and breathe. A cardiology patient simulator named Harvey, developed by Michael Gordon in 1968 at the University of Miami Medical School, featured pulses, blood pressure and heart sounds (the latest model is still in use).
By the late 1980s and early 1990s, smaller, more powerful computers led to exponential leaps in simulation technology. Among a new generation of pioneers was David Gaba, then a young anesthesiologist at Stanford University. “I was a big aviation buff as a kid, and I’d known about simulators for a long time,” says Gaba, who is now the associate dean for Immersive & Simulation-Based Learning at Stanford. “Putting a patient under anesthesia is intrinsically hazardous—just like taking a plane up. Things happen in seconds, minutes and hours, not days, weeks and months.” In 1987, Gaba and his team introduced the first of a series of simulators known as CASE (comprehensive anesthesia simulation environment). About the same time, a University of Florida team created its own anesthesia simulator.
Today there are hundreds of simulation centers around the world, compared with fewer than 20 a decade ago, according to James Gordon, a Massachusetts General Hospital emergency physician who directs the Gilbert Program in Medical Simulation at Harvard Medical School. Yet simulation training plays only a small role in most students’ education—in part because the cost of simulators, ancillary gear and expert instructors can strain training budgets. (Medium-capability simulators cost up to $50,000.) Gordon believes prices will drop as simulators become more widely used, and whereas today Harvard Medical School students may train on simulators a few times a year, he foresees a day when such training will become routine.

GORDON TAPES SIMULATOR SESSIONS SO medical students can review their performances. On one such tape, four novices are working anxiously to figure out how to help their mechanical patient breathe after a morphine overdose. Though the patient could easily have been revived with Narcan, a readily available drug that counteracts the effects of narcotics, none suggests it. “All of them would have gotten it right on a written test,” Gordon says.
Such training blunders could become real tragedies a few years later when young residents find themselves flying solo for the first time. “Most errors occur early in a doctor’s career—in her first 10 cardiac catheterizations, or his first 20,” says Steven Dawson, a Massachusetts General Hospital interventional radiologist who now directs simulation research at the Center for the Integration of Medicine and Innovative Technology (CIMIT). Based in Cambridge, Mass., the medical technology partnership links several Harvard-affiliated hospitals and the Massachusetts Institute of Technology. Looking back on his own training, Dawson expresses a common frustration—that his hands-on experience was limited to cases that happened to present themselves. “If you came in and you needed a procedure, I learned on you,” Dawson says. “If a given disease or injury didn’t come through the door, I didn’t see it.”
Nor do young doctors typically get much practice working as part of a group under fire, when an individual is most error-prone. Physicians, nurses and technicians may talk over one another and miss key messages; they may intimidate or be intimidated by those below or above them in the medical pecking order. Jeffrey B. Cooper, director of biomedical engineering for Partners Healthcare System, thinks that by training together in simulated emergencies, groups can recognize trouble signs and work to prevent them from being repeated when lives are on the line. In addition, the training can help foster a culture in which clinicians feel comfortable critiquing their own performances.
A mentor to Stanford’s Gaba, Cooper has been studying simulator training methods since the late 1980s. He now heads the Center for Medical Simulation, which regularly hosts groups of practicing anesthesiologists, obstetricians, physicians from other specialties, nurses and emergency medical teams. They work in facilities like operating rooms and critical-care units that, except for the mannequin lying prostrate on the bed in lieu of a patient, are realistic down to the final detail. There are clamps and bottles of medication, surgical gloves, even boxes of Band-Aids. “We believe people will learn best if it feels real to them,” says Cooper, who is also a biomedical engineer in the Massachusetts General Hospital’s department of anesthesia and critical care. “They’ll buy in if they can relate it to their real work.”
A FEW DOORS DOWN FROM Cooper’s office at CIMIT, Dawson’s team seems determined to simulate every kind of clinical conundrum. Tapping the keys of his computer, Dawson calls up an X-ray of a human skull. Though sharp and clear, the image seems ordinary until he reveals it’s not an actual skull but one created artificially using mathematical calculations.
“I’m a radiologist, and I can’t tell the difference between that and a real X-ray,” Dawson says. With a few keystrokes, the cranial cavity fills with a network of blood vessels that are then suffused with a contrast medium, as though injected to pinpoint carotid disease. Next, a catheter snakes to the brain. A few more strokes and the image rotates, displaying the skull and vessels from every angle. What had been a static X-ray image blossoms to three-dimensional life.
But what really excites Dawson are simulators that combine such on-screen wizardry with tactile realism. The Vascular Intervention System Training, or VIST, lets physicians re-create a patient’s veins, arteries and tissue, and then practice threading a catheter through this anatomically identical system contained in a rectangular box. Developed by members of Dawson’s team in collaboration with Japanese electronics giant Mitsubishi, VIST feeds information to a display monitor, which helps doctors guide the catheter along its circuitous route.
Another system, VIRGIL, is designed to train medics to diagnose and treat battlefield chest wounds. Working on a life-size model developed by and for the U.S. military just before the terrorist attacks on Sept. 11, 2001, a physician preps an area with Betadine (an antibacterial solution), cuts a hole, inserts a clamp and then sweeps a finger inside to make room for the tube. When the tube goes in, there’s a rush of either blood or air, depending on the type of injury the computer randomly selects. Push in too far and damage the liver—a relatively common error among inexperienced medics in the heat of combat—and the computer announces, ominously, “You’ve killed the soldier. Do you want to try again?”
Dawson demonstrates another simulator, a fleshy cylinder with the heft and density of a Marine’s muscular arm that duplicates the difficulties of administering a smallpox vaccination, a surprisingly delicate procedure. (One pokes lightly at the skin using a small instrument with two pointed tips like a miniature fondue fork.) Proper vaccination produces a faint bloom of blood. Excessive bleeding, or none at all, means you’ve done it wrong. Dawson jabs at the arm and watches with satisfaction as tiny red dots appear on the surface.
Dawson’s team is working toward one of the holy grails of simulation technology: a synthesized, full-size model whose materials and software enable it to reflect and reproduce almost any system or condition of an actual human body. “I don’t believe in virtual reality,” Dawson says. “I believe in real reality.”
But others envision a future in which mannequins are replaced by 3-D imaging so sharp that physicians-in-training actually “feel” the patients they are treating in a computer-generated operating room. “Mannequins have their place, but as 3-D reality becomes more and more sophisticated, our need for them is likely to diminish,” says Jeffrey Taekman, director of the Human Simulation and Patient Safety Center at Duke University.
The idea of learning in a virtual world seems natural to many of today’s students. “Most have been raised on computers and rapid-fire multimedia,” says Taekman. “They are a new age of learner. They’re comfortable with all kinds of computer resources, and that’s how they prefer to get their information.”
But virtual or not, patient simulators are going to become a ubiquitous presence in medicine, predicts Cooper, who foresees myriad devices and approaches suited to an equally vast array of needs. “A generation ago people questioned whether computers would ever have a place in medicine,” Cooper says. “Now they’re so common you don’t even think about them—you just realize the benefits. That’s where simulators are headed.”
Dossier
“A Brief History of the Development of Mannequin Simulators for Clinical Education and Training,” by J.B. Cooper and V.R. Taqueti, Quality & Safety in Health Care, Oct. 2004. An excellent grounding in the history of simulators.
www.thesimgroup.org The next best thing to playing with them: detailed descriptions and demonstrations of VIRGIL and other simulation devices being produced at The Sim Group.
“The Future Vision of Simulation in Health Care,” by David Gaba, Quality & Safety in Health Care, Oct. 2004 (Supplement 1). One of the pioneers of modern simulation offers his outlook on the field’s future.
Stay on the frontiers of medicine
Related Stories
- Simulators Surge
High-tech mannequins and simulation software are becoming more prevalent in medical schools.