Published On July 23, 2009
EVER SINCE 1973, WHEN A RESEARCH TEAM IN CALIFORNIA—led by Stanley Cohen at Stanford and Herbert Boyer at the University of California, San Francisco—introduced foreign DNA into a bacterium, thus creating the first genetically altered organism, scientists have been devising remarkable techniques in what came to be known as genetic engineering. From that beginning, an entire industry—biotechnology—has sprung, as has the promise, and often the reality, of lifesaving, paradigm-shifting therapies. But the work of genetic engineers, long at the forefront of biomedicine, has come to seem almost plodding to some scientists.
Genetic engineers typically work with just one gene, proceeding by trial and error in a process that’s as much art as science. And they use tools that haven’t changed much since the early days, when they learned how to snip a piece of DNA from one organism, such as a mouse, insert it into a virus or other “vector,” which delivers it into another organism—a worm, say—and then observe what happens. Or they alter a gene from a mouse to study that gene’s function—extrapolating by observing what occurs when the gene isn’t working. That capability alone has spawned generations of “knockout” animals (a gene’s function is “knocked out”) that are used to better understand the role of genes in disease and to test treatments.
But now, says James Collins, a bioengineer at Boston University, “many engineers don’t consider genetic engineering to be engineering. They view it more as, say, replacing a red lightbulb with a green lightbulb.”
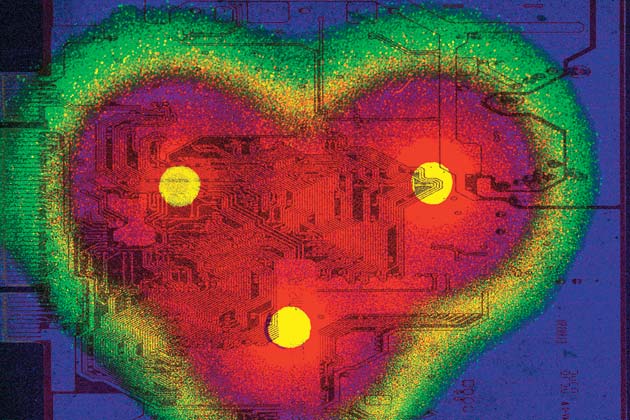
Collins prefers to manipulate the underlying wiring, operating in the realm of synthetic biology, where researchers may add entire “circuits” of genes, often taken from several species, into a single organism. The genes in the circuit interact; one gene may turn another on or off, depending on the environment, and the second gene may then affect the third and so on. Or each gene may produce a protein needed to achieve a desired outcome—making a complex drug, for example. These gene circuits are often added to yeast or to the bacterium E. coli (which provides the energy and raw materials) to make those microorganisms perform complicated, prescribed functions—in a sense, as microscopic factories.
Almost 10 years ago, Collins wondered whether a simple cell could become a primitive computer. Computer code is based on the binary system, with every piece of information reduced to a series of zeros and ones. Attempting to create a similar on/off mode for E. coli, Collins came up with a kind of toggle switch, a pairing of genes, each of which produced a protein that turned the other gene off; they couldn’t both be on or off at the same time.
“The toggle switch is just a simple form of memory,” says Collins, who in 2004 reported that he had programmed E. coli cells using a similar toggle switch to “remember” events, such as DNA damage to the cells, using the toggle switch’s on/off positions, which work like a computer’s binary code. When radiation, for instance, strikes the DNA, the switch turns on one of the bacterium’s genes, and that causes the other gene to turn off permanently, thus committing the event to a cell’s binary memory even if there’s no more DNA damage for the life of the cell. What’s more, because the second gene Collins used also represses the action of a gene he added that produces green fluorescing protein, turning off the first gene enables GFP to turn on—and its green glow serves as a visual clue that the cell’s DNA has been harmed.
This sort of work could be useful for making bacteria respond to a change in their environment. For example, Collins linked the toggle switch to a gene that triggers the formation of a biofilm, a complex grouping of bacteria that protect the E. coli cells against further damage from the destructive agent that attacked their DNA. Other researchers are using synthetic biology to create cheap fuel from microbes, to eliminate the growing resistance of bacteria to antibiotics, and to build drug factories inside yeast cells, so they can replicate natural processes but at a fraction of the cost of typical drug production.
In describing their work, synthetic biologists are forthright about their goal of taking control of biological processes, of using their knowledge about how life forms are constructed to improve on what some have termed nature’s “inelegant” solutions. They think they can make cellular “machines” that do things unaltered cells cannot, and instead of Darwin’s evolution and natural selection, they talk of directed evolution and artificial selection. In a sense, synthetic biology is what genetic engineering has evolved into.
All of this is very new, and much of it remains the most basic of basic science, teaching researchers who are trying to manipulate natural processes a lot about those processes themselves. But Collins and other scientists from wide-ranging disciplines are already moving down the road from the theoretical to the practical, and their progress to date suggests that if the potential of synthetic biology is realized, their inventions could rival the astonishing feats genetic engineers have accomplished over the past 30 years.
IN TRADITIONAL GENETIC ENGINEERING, RESEARCHERS INSERT a single gene into a small circle of DNA, called a plasmid, and add a sliver of DNA, called a promoter, that turns the gene on or off. They then inject the whole thing into a model organism, such as a mouse or a bacterium, altering its genetic makeup. But Jay Keasling, a pioneer of synthetic biology at the University of California, Berkeley, prefers to develop promoters that act more like dimmer switches than on/off buttons, allowing him to slowly turn genes up or down, making a little bit more or less protein. He has invented tools that let him control multiple genes simultaneously, and he’s created a new kind of molecular scaffolding that tethers the genes in a circuit so that the reactions happen much more quickly and efficiently than if the genes were floating randomly in a cell.
Initially, these were tools without a particular purpose. But then Keasling and his colleagues put them to work in manipulating a family of molecules called isoprenoids. Cholesterol and carotenoids (such as beta-carotene, which makes carrots orange) are isoprenoids, and the family also includes such powerful drugs as Taxol (paclitaxel), for chemotherapy, and artemisinin, used to treat malaria. Although many strains of the parasite that causes malaria have evolved resistance to such standard antimalarial drugs as quinine, artemisinin remains effective. But it’s very expensive and labor-intensive to produce in a process that extracts small amounts from the wormwood plant, a tall, leafy herb that grows in temperate regions of Asia. Building on the work of others who had figured out an important step in the process, Keasling’s group set out to create an alternative means of production.
Producing the drug quickly and inexpensively in a microbe could make it available to many of the 300 million to 500 ?million people, almost all in developing countries, who suffer from malaria. In 2003, Keasling published a paper showing how to convert sugar, through multiple chemical transformations, into amorphadiene, a precursor to artemisinin. He did it by inserting eight genes that encoded eight different enzymes into the E. coli bacterium. Some of the genes came from E. coli(they were engineered to express much more protein than they normally would), while others came from yeast, and one from the wormwood tree, altered to make it similar to an E. coli gene and to produce higher levels of amorphadiene. The eight enzymes produced by the inserted genes catalyzed the reactions changing acetyl coenzyme A (from sugar) into each of the intermediate molecules on the pathway to amorphadiene. Thus altered, the E. coli cell became a tiny chemical factory.
But Keasling’s group was still a few steps from making the drug itself. So the team looked for genes in plants related to wormwood, such as sunflower and lettuce, which produce molecules similar to artemisinic acid and are like the genes in wormwood. Finding and understanding those genes helped the researchers narrow their search for the genes in wormwood, which would complete the final stages for making artemisinin. They added those genes to yeast (a “chassis” organism for making the drug industrially) and converted amorphadiene into artemisinic acid, which is easily converted to artemisinin. The hope is to suspend the genetically altered yeast in a 50,000-liter fermenter filled with a sugar solution and thus to mass-produce artemisinin. Keasling is working with drugmaker Sanofi-Aventis to create a manufacturing process that could substantially reduce the cost of artemisinin, making the drug affordable to the millions who need it. ?“There may be other drugs, including HIV therapies, that could be produced at a greatly reduced cost using a similar process,” Keasling says.
EVEN IF SYNTHETIC BIOLOGY RESULTS IN THE INEXPENSIVE manufacturing of artemisinin, malarial parasites are likely to evolve defenses against the drug, gradually reducing its effectiveness. Drug resistance is already a problem for most classes of bug-fighting pharmaceuticals, and it has become especially acute in the case of antibiotics, which typically kill bacteria by damaging their DNA, using molecules called hydroxyl radicals (oxidation). The bacteria respond by activating something known as the SOS pathway to repair the DNA damage, and the more they’re exposed to a particular drug, the more adept the pathway becomes at fighting off the antibiotic’s attack. The gene lexA3, which is naturally found in E. coli, represses the SOS pathway, and Collins, the bioengineer at Boston University, has focused on dramatically increasing production of lexA3 as a way to break down resistance to antibiotics and increase their potency.
Collins inserts the gene into tiny viruses called bacteriophages and uses PltetO, a synthetic, off-the-shelf promoter, to make the bacteriophages produce multiple copies of the gene. The bacteriophages carry these genes into a targeted bacteria that, Collins has found, boosts the effectiveness of antibiotics and increases the survival of infected mice. He even hopes that bacteriophages, added to apparently defunct antibiotics, might bring the drugs back to life. “In many cases of resistance, it’s still possible for the antibiotics to kill the bacteria; it’s just that the drugs don’t kill as effectively at the concentrations that are typically used,” he says. “This should make them more effective by blocking the bacteria’s defense pathways.”
In contrast, Christopher Anderson, a synthetic biologist at UC Berkeley, has learned to make bacteria more lethal, though in a very precise, highly targeted way. He creates microbes that, when injected into the body, home in on a cancer tumor and kill it. To achieve this, a bacterium must identify the field of battle, whether it’s the bloodstream or inside a cancer cell itself, and act accordingly. And it must avoid ejecting its killing solution—which could be enzymes that chew up the tumor’s DNA or molecules that activate cell suicide (apoptosis)—in the wrong place.
To accomplish all this, Anderson inserted a series of genes for sensing and reacting into E. coli and encased the bacteria in a carbohydrate shell. That way they won’t be attacked by the body’s immune system. “If you just take naked E. coli and stick it into a mammalian bloodstream, it gets cleared in under five minutes,” Anderson explains. “The carbohydrate shell makes it look like something that’s supposed to be in your body, something that is not a bacterium.”
Anderson also altered genes in the bacteria, a few whose protein causes inflammation and others that stop the bacteria from growing and reproducing. Once injected, the bacteria find their target through a complicated series of events triggered by the special environment of a tumor. Blood vessels in tumors are highly porous (more so than anywhere else in the body), enabling the bacteria to slip from the bloodstream into the tumor. There, programmed to detect the low oxygen levels that characterize tumors, a promoter called fdhF that researchers inserted in the bacteria turns on a gene associated with the protein invasin. Invasin causes the cancer cells within the tumor to take in the bacteria. Inside the cancer cell, the bacteria sense another unique environment, the absence of magnesium and iron, which switches on a gene in the bacteria that pops them open, releasing enzymes that attack the cancer cells’ DNA or another chemical that kills the cells.
Anderson hopes that someday this process can deliver a message to the cancer cells to undergo apoptosis, thus stopping their uncontrolled proliferation. And though he has so far published only one part of this engineering scheme—regarding invasin’s role—he is preparing papers on the other aspects. Testing the process in mice is next, and he’s also working on engineering bacteria to target specific types of tumors—for example, by using breast cancer–related proteins to force cells in breast tumors to take in bacteria that will be lethal to the tumors.
Of course, working with living cells and systems is far different from engineering machines from steel or polymers, and Boston University’s Collins notes that researchers in this burgeoning field must learn to live with a level of uncertainty, knowing that their creations literally have lives of their own. In a new paper, he describes how he has gotten microbes to count—to three. Such a living calculator might be useful if, say, a researcher wanted to program a cell to die after a certain number of divisions so that it wouldn’t grow out of control. That could act as a safety mechanism in engineered microbes used for medical purposes, so the microbes wouldn’t outlive their usefulness. But even then, there will be limits, Collins says: “I don’t think we will ever achieve complete control over living organisms. They are too complex. However, I think we can achieve some level of control, modifying their functions and altering behaviors in beneficial ways.”
Dossier
“Synthetic Gene Networks That Count,” by Ari Friedland et al., Science, May 29, 2009. James Collins and colleagues demonstrate how they transformed the E. coli bacterium into a crude computer, genetically encoding it to count to three.
“Production of the Antimalarial Drug Precursor Artemisinic Acid in Engineered Yeast,” by Dae-Kyun Ro et al., Nature, April 13, 2006. Researchers show how to coerce yeast into converting sugar into the raw material for a powerful antimalarial drug.
The Registry of Standard Biological Parts. The BioBricks catalogue, in which researchers (or anyone) can browse virtual shelves of biological “parts,” which they can order and assemble into new genetic systems for a cell.
Stay on the frontiers of medicine