Published On August 11, 2022
Harland Winter, a pediatric gastroenterologist at Massachusetts General Hospital, clearly remembers the day in 2010 when he received an email from Mauro Toporovski, a pediatrician in Sao Paolo, Brazil. Toporovski sought Winter’s advice about an infant girl named Nechama who had a mysterious case of severe, intractable diarrhea. Although Toporovski had tried switching her from breast milk and cow’s milk formula to soy-based formula, the diarrhea persisted. Tests showed that Nechama was losing a significant amount of protein in her stool.
To find the cause of the baby’s gastrointestinal distress, Toporovski had run every exam he could think of, including a screening for congenital diarrhea disorders, which are relatively rare. He consulted with several colleagues in Brazil and beyond, including Winter. But no one could figure out what was wrong with the child.
When Nechama was 17 months old and still hospitalized, she acquired a serious infection, most likely because her immune system was weakened by malnutrition. She developed sepsis, possibly related to the catheter she needed for nutrition, and died.
A month later, Nechama’s mother was pregnant. Toporovski offered congratulations, but he was worried that the little girl’s diarrhea might have had a genetic cause, a mutation that the new sibling could also inherit. “I hoped that it was just one case, and that the other baby would survive and be healthy,” says Toporovski. But after a trouble-free pregnancy, the woman gave birth to a boy, Eliashiv—and he also developed severe diarrhea. “It was exactly the same disease,” says Toporovski.
Winter agreed that the diarrhea probably had a genetic cause, and to help identify it, he consulted Mark Daly, the founding chief of the MGH Analytic and Translational Genetics Unit, launched in 2010 by the department of medicine to connect clinical researchers at the hospital with the burgeoning world of genomic medicine. “Genome sequencing was then still in its very early days,” says Daly, who had recently begun using the technology to conduct clinical research with colleagues at the Broad Institute of MIT and Harvard. “We were building new tools in real time.”
One of those tools was whole-exome sequencing, a process that scans the exome, the 1% or so of the human genome that carries the code for making proteins. Most known gene mutations associated with diseases occur in these regions. Daly recommended using this process to search for a potential genetic cause of the syndrome that had killed Nechama.
Winter requested blood specimens from Eliashiv, both parents, an older brother who had never developed chronic diarrhea and several other relatives. He was also able to get a sample of Nechama’s blood, preserved from birth in the form of a “blood spot,” a tiny amount of blood taken from a newborn’s heel for routine screening and collected on special paper.
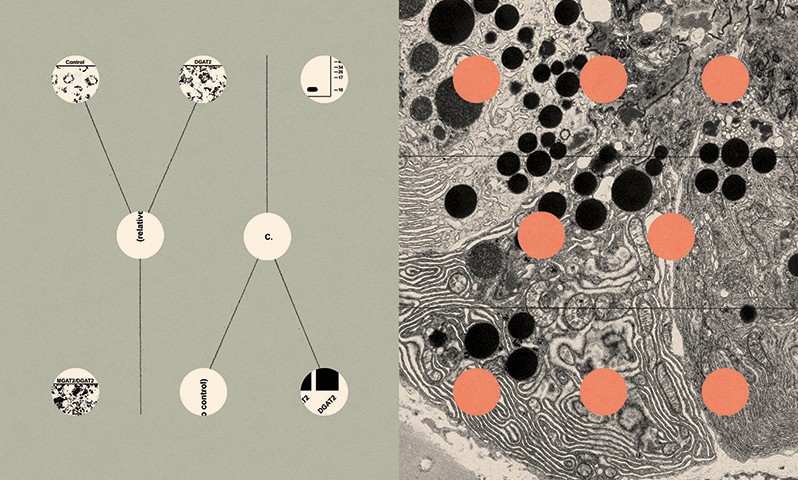
Daly, working with Christine Stevens, now an associate director of scientific projects at the Broad, oversaw extraction and sequencing of DNA from the blood specimens. They discovered that each parent had one normal version (or allele) of a gene called DGAT1, as well as a mutant allele that suggested they were missing a segment known as exon 8. Someone who has both a normal and a mutant version of an allele—making that person heterozygous, in scientific terms—shouldn’t have problems, because the normal gene is able to provide code for making an essential protein. Babies, however, receive one allele from each parent, and Nechama and Eliashiv were both homozygous for the DGAT1 mutation—each child had inherited two copies of the mutant gene.
This was compelling evidence that the DGAT1 mutation might be behind the children’s life-threatening diarrhea. But the researchers needed to know more—about the role of a normal DGAT1 gene, and why its absence might make babies so sick. The search for answers led Winter, Daly and the others to a laboratory 3,000 miles away, where other scientists were already working to solve the mystery of DGAT1—a mutation that not only caused the rare illness but seemed to play a critical role in the way that the body metabolizes fat.
Physician Robert Farese Jr., in his laboratory at the Gladstone Institutes at the University of California, San Francisco, had focused much of his research on cellular lipid metabolism, and in 1998, Farese and his colleagues identified a gene that produces diacylglycerol O-acyltransferase, or DGAT. It’s an enzyme that converts fatty acids from food into triglycerides, a form of fat stored by the body in lipid droplets to produce energy. A short time later, collaborating with a biotechnology partner, Farese’s lab discovered a second form of DGAT. The researchers first found it in plants but then discovered it was present in humans, too. Two genes, DGAT1 and DGAT2, carried the code for these enzymes.
Farese and his colleagues observed that mice bred not to have the DGAT1 gene—and thus not producing the DGAT1 enzyme—had remarkable qualities. “Those mice looked amazing,” says Farese. “They were thin, didn’t get obese and lived 25% longer than other mice.” The mice also seemed impervious to metabolic conditions such as diabetes and nonalcoholic fatty liver disease, a condition that affects about one in four U.S. adults. For those involved in the research, as well as the pharmaceutical industry, this discovery looked like a breakthrough that could have far-reaching implications. Being able to replicate those effects in people could improve health and save millions of lives. Several companies began to develop and test experimental compounds that blocked or inhibited DGAT1 as potential treatments for obesity, elevated triglycerides and other conditions.
MMice bred not to have the DGAT1 gene had remarkable qualities.
In July 2011, Daly emailed Farese to say that the whole-exome sequencing of Nechama and her family had identified a mutation in DGAT1 that appeared to be linked to severe diarrhea in children. By then, Farese had established a joint lab with biochemist Tobias Walther, which they would transfer to the Harvard T.H. Chan School of Public Health in 2014. Farese, Walther and their team produced a clone of the DGAT1 mutation Daly had discovered and tested it in the lab. “We found that there was a total loss of DGAT activity,” says Farese. That explained why babies who lacked the DGAT1 enzyme developed gastrointestinal distress. Without enzymes to make triglycerides that can be stored in lipid droplets, fatty acids from food build up in the intestine “and wreak havoc,” says Farese. The accumulation of these detergent-like compounds damages cell membranes and promotes cell death, resulting not only in diarrhea, vomiting and other GI symptoms, but also dangerous loss of protein in the stool. That was also the reason that those DGAT1-blocking drugs, developed with high hopes for treating obesity and other metabolic conditions, haven’t worked in people. While it’s not clear why mice without DGAT1 avoid the problems that are so debilitating in people, Farese suspects it may be because mice, unlike humans, also make DGAT2 in their intestines, and that related enzymes can serve as a back-up mechanism for turning fatty acids into triglycerides.
The emerging understanding of how and why DGAT1 deficiency led to GI symptoms meant there might be a straightforward solution for people with the mutation—simply reduce fat in their diet. Eliashiv had been fed formula through a vein, which bypassed the gut and kept him alive. But when he was placed on a fat-restricted diet, his diarrhea soon eased. He gained weight and was discharged, and today, he’s a healthy 10-year-old. It’s only when he consumes dietary fat, says Toporovski, that the diarrhea comes back.
A Key to the Body's Fat?
THE ROLE OF DGAT2 COMES INTO FOCUS.
Robert Farese Jr., who helped pioneer research into the enzymes DGAT1 and DGAT2, and Tobias Walther are probing the mysteries of lipid droplet biology at their joint laboratory at the Harvard T.H. Chan School of Public Health. Some of that work has focused on DGAT2. It turns out to be essential for making triglycerides, which provide storage for most fat in the body. Farese and Walther recently made an intriguing discovery in animal studies. “When you block DGAT2, you shut down not only production of triglycerides but also lipid synthesis in general,” Farese says.
The scientists theorize that the body may have a feedback loop, wherein the amount of fat stored influences how much fat is made, and vice versa. “That would be fundamentally exciting to understand,” says Farese. “But it could also be exciting from a therapeutic standpoint. With a DGAT2 inhibitor, it appears that you not only block triglyceride synthesis; you also shut down the production of new fat. That could be quite an effective drug.”
The most promising use of such a therapy would be to treat nonalcoholic fatty liver disease, which affects about one in four Americans and can lead to liver failure. A drug that blocks DGAT2 synthesis is currently in development. In a randomized trial, patients who received the experimental drug experienced a rapid and large drop in liver fat, compared with no change in patients who got placebo shots.
Farese and Walther also continue to study other aspects of the basic biology of lipid droplets, and working with colleagues at the Broad Institute of Harvard and MIT, they recently unveiled the Lipid Droplet Knowledge Portal (lipiddroplet.org), an open-source repository for research on the genomics and proteomics of these complex, critically important structures.
In 2012, the team of clinicians and scientists who linked the DGAT1 mutation to congenital diarrhea reported their findings in the Journal of Clinical Investigation (JCI). The paper noted that although the mutation is extremely rare, it had been found in at least seven members of a family of Ashkenazi Jewish ancestry—Nechama and Eliashiv, who were homozygous for the DGAT1 mutation, as well as their older sister, parents and two grandparents, who carried only one copy of the defective gene and were unaffected.
Most Ashkenazi Jews are descended from a relatively small population in Eastern Europe, and many choose to marry within their faith and community, increasing the chance that a child might inherit a disease-causing gene mutation from both parents. Conditions such as Tay-Sachs disease, Gaucher disease and others are more common among Ashkenazi Jews because of this kind of genetic concentration, and most babies known to have been born with the DGAT1 mutation have had Ashkenazi Jewish ancestry, says Daly. He estimates that one to two of every 100,000 children born in this community are homozygous for the defective gene, compared with perhaps one in 100 million worldwide.
Although most children diagnosed with DGAT1 deficiency have the same mutation in the DGAT1 gene—the one that causes a “skip” of exon 8—physicians and researchers have found that there are other mutations in the same gene that can also cause problems. One of those came to light in 2012 in London. Twin boys, Rishaan and Kiaan, developed diarrhea and vomiting immediately after birth, landing them in intensive care for three weeks before they were sent home. But their GI distress didn’t respond to treatment and the boys were in and out of hospitals for the next two years as they got sicker and sicker. Their doctors didn’t expect them to live.
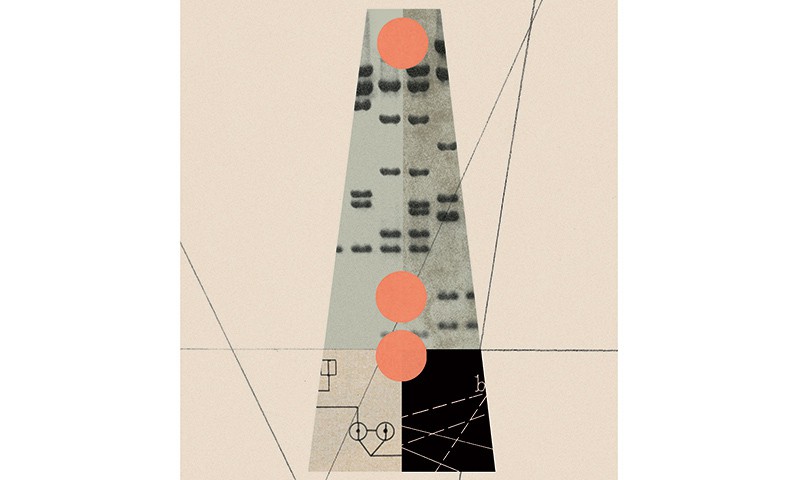
So the parents took their sons to Columbia University Medical Center in New York City, where doctors initially suspected they had mitochondrial disease. When tests proved that theory wrong, geneticists at Columbia suggested that DGAT1 deficiency might be the cause and proposed performing whole exome sequencing for the twins and their parents.
Both boys had developed an aversion to eating, and Kiaan was so ill he couldn’t stand. His father brought him to Boston Children’s Hospital, and Winter at MGH was consulted. “At that time, DGAT1 deficiency had been identified only in children of Ashkenazi Jewish descent,” says Nina Gluchowski, who was a pediatric gastroenterology fellow at Children’s when the boy arrived and went on to work in the Farese and Walther lab. “We didn’t know whether it was even possible that other children might be affected by the same condition,” as the family is of Indian ancestry.
Sequencing revealed, however, that the twins were homozygous for a DGAT1 mutation that was different than the gene variant found in Ashkenazi Jewish children. Yet this mutation, too, seemed likely to cause GI distress, and Kiaan was immediately placed on intravenous feeding. Two days later, as his father sat next to his hospital bed eating steamed edamame, the boy reached over, snatched a handful of the soybeans and gobbled them. “He didn’t stop eating for two weeks,” says Rishi, whose son craved egg whites, more edamame and other foods. “It was like a miracle.”
Winter saw the need for a simple blood test that could detect the DGAT1 mutation.
The family soon returned to London, and the twins were put on a diet of foods such as plain chicken, rice, potatoes and edamame. Today, they’re energetic 10-year-olds who excel in school and love sports. Gluchowski worked with Farese and Walther in the lab at the Harvard School of Public Health to determine how this mutation functioned. It turns out that, unlike the mutation in the Ashkenazi children, this mutation allowed both boys to tolerate a modest amount of fat in their diets, apparently because the novel DGAT1 mutation they were born with causes only partial loss of the DGAT1 enzyme. “We now know that DGAT1 deficiency seems to be more of a spectrum of disease,” says Gluchowski, now at the University of Vermont Medical Center. She notes that some children with the deficiency can tolerate up to 10% of calories from fat. What’s more, children born without the ability to make adequate amounts of the DGAT1 enzyme may compensate by ramping up activity in their DGAT2 genes, according to one theory.
DGAT1 deficiency is a rare disease, and what scientists have learned about DGAT1 mutations has been crucial in helping a small number of children born with the gene variants. Since first working with Mauro Toporovski in Brazil, Winter has treated or consulted on many cases of congenital diarrhea linked to DGAT1 mutations. But most of these cases were discovered only after babies had already gone through months or years of extreme, life-threatening distress. The whole exome sequencing needed to confirm a diagnosis could take up to two months to produce results. Early on, Winter saw the need for a simple blood test that could detect the DGAT1 mutation more quickly.
He turned to the Laboratory for Molecular Medicine at Mass General Brigham (then Partners HealthCare) to develop one. The scientists there developed an assay that can determine within a few days whether a baby has the Ashkenazi mutation. (Blood panels that screen for multiple DGAT1 mutations are now also available.) This assay would enable early diagnosis and make possible the prevention of severe manifestations of DGAT1 deficiency.
In 2021, Winter heard from a mother who had a child with the DGAT1 mutation. She said that she was pregnant again and asked for his help in case the new child developed the same problem. Indeed, a baby girl, born in January 2022, had mild symptoms while being fed breast milk. When the assay for the DGAT1 mutation quickly confirmed that she was homozygous for the Ashkenazi gene variant, the parents brought the baby, then just eight days old, to MGH. Clinical nutrition specialist Jill Israelite oversaw her feeding of a special formula without fat, which was developed by Peri Milman at Hadassah Hospital in Jerusalem. The baby’s condition improved enough during the first week for her to be transferred to Columbia Medical Center, closer to the family’s home.She was discharged a few weeks later and is now faring well on a special fat-free infant formula with intravenous fat supplementation. Early detection and treatment enabled her to avoid the severe diarrhea and protein loss caused by a deficiency in DGAT1.
That little girl, like Eliashiv in Brazil and Rishaan and Kiaan in London, is fortunate in finding a treatment for the condition. As with most rare diseases, families and children with DGAT1 deficiency struggle to find resources. Harland Winter credits the advances in discovering this new disease, identifying a treatment, developing early diagnosis and, after only 10 years, being able to prevent symptoms to “the efforts of health care providers, scientists and parents who worked together to improve the lives of children,” he says.
Dossier
DGAT1.org. The website, with medical information from Harland Winter and his colleagues, serves as both a primer and support group for families and caregivers of children with DGAT1 deficiency. It was founded by Dia Khosla, the sister of twins born with the condition.
“DGAT1 Mutation Is Linked to a Congenital Diarrheal Disorder,” by Joel T. Haas et al. The Journal of Clinical Investigation, December 2012. The first report on the extremely rare gene mutation links the condition to severe diarrhea and other symptoms in newborns.
“An Introduction to Lipid Droplets,” by Robert Farese Jr., and Tobias Walther. In this three-part iBiology.com podcast, two Harvard scientists and leading experts on DGAT1 explain how the body uses this enzyme and other factors to make fat.
Stay on the frontiers of medicine
Related Stories
- The Search for a Regeneration Switch
Can studying salamanders and spiny mice help humans grow new limbs? Answer: It’s complicated.
- Four Breakthroughs That Led to the Pig Heart Transplant
Taking organs from another species and making them work in humans is potentially a quantum leap in medicine. Here’s a summary of what got us there.
- The Insomnia Genes
Poor sleep affects almost half of the country, and solutions have been hard to come by. Tracing the problem to its genetic roots may stop the tossing and turning.