Published On January 15, 2014
IT’S A SCENE REPEATED COUNTLESS TIMES every day in hospitals across the country. A patient lies in bed, hooked up to tubes, unshowered, in a hospital gown. Awakened every few hours during the night for medicine or tests, she has gotten little sleep. Her elderly husband has gone home to rest, and now she feels nauseated, weak and scared. She’s unsure exactly what is wrong with her.
Then a physician, on her morning rounds, comes in. She seems caring and well meaning as she asks the patient how she is feeling. She shares lab results, discusses the diagnosis and explains what comes next. The patient listens, and nods whenever the doctor asks, “Do you understand?” After several minutes, the doctor moves on to the next patient, satisfied that she has done her job.
Yet research shows that many patients, especially those who are old, sick or less educated, don’t understand, even when doctors are sure that they do. They lack “health literacy,” a concept that goes beyond patients’ ability to read, write and handle numbers to encompass having the capacity to understand and deal with matters relating to their own health. “There’s a series of skills patients must have every time they encounter the health care system,” says Stacey Sheridan, a researcher at the University of North Carolina. “It starts with making an appointment, and it continues with finding your way to the visit, checking in, filling out all kinds of forms, talking to the doctor, and getting follow-up testing.” That’s on top of being able to grasp complex scientific terms and issues, analyze medical information, and apply that knowledge. To be truly health literate, you also need to be able to put your condition into context, understand what influences it, and grasp how you may need to change your behavior.
It’s believed that about one in five U.S. patients has low health literacy, while roughly 30% more qualify as marginally literate. (Researchers peg patients’ statuses to traditional educational levels, with low literacy equating to a sixth-grade understanding or below, and marginal literacy being what a seventh or eighth grader might be expected to have.) And some researchers believe that as many as two out of three older patients have a level of literacy that leaves them unprepared to find their way through today’s complex medical system.
When inadequate health literacy hinders patients in managing their own care, their health may suffer and costs often rise. Study after study has shown that low health literacy is associated with higher hospitalization rates, more ER visits, and a lower likelihood of receiving preventive care such as mammograms and flu shots. A 2012 study at Boston Medical Center, for example, showed that patients with low health literacy were almost twice as likely as others to return to the emergency department within 30 days of an initial visit.
And problems with health literacy can lead to a cycle of unwanted consequences. Many patients don’t have a clear understanding of their illness or of how to manage it effectively. Physicians regularly overestimate how much patients comprehend and make matters worse by sprinkling their explanations with jargon. And the increasing complexity of medication regimens and other aspects of care that patients are expected to manage on their own, often by navigating online resources, makes it all the more likely that their health will be affected. They often remain unwell or suffer relapses, and in the process they cost the health care system a lot of money. A recent broad push toward shared decision making—the idea that patients should be partners with physicians in directing their own treatment—runs smack into the reality that many patients lack the health literacy that such participation requires.
PHYSICIANS CONSISTENTLY OVERESTIMATE their patients’ level of health literacy. In a randomized controlled trial in 2005, researchers at the University of California, San Francisco wanted to test whether telling doctors about a patient’s limited health literacy altered the way the physician interacted with that patient. At an urban, academic public hospital, they screened 441 patients with type 2 diabetes for health literacy using the standardized short form of the Test of Functional Health Literacy in Adults (s-TOFHLA). Based on those results, they chose 182 patients with low scores and then divided the primary care physicians of those patients into two groups, only one of which was told about the patients’ limited health literacy. The researchers found that physicians notified of their patients’ limited health literacy had originally overestimated health literacy in 62% of their patients (the real-world result being that they often miss the opportunity to take steps to improve the situation).
In such studies, researchers can use s-TOFHLA or other tools to diagnose patients’ health literacy. That test gauges whether patients can read such things as the labels on prescription bottles by asking them to fill in missing words. Another standard research questionnaire—REALM, for Rapid Estimate of Adult Literacy in Medicine—scores patients’ ability to read and pronounce common medical words, usually a list of 66 in increasing order of complexity (from “eye” to “antibiotics”). But that process is anything but rapid, and neither REALM nor s-TOFHLA is practical in the clinic, where caregivers don’t have sufficient time during a rushed office visit to use the tools.
There might, however, be time to ask a single question, and Lisa Chew, associate professor of medicine at the University of Washington, and her colleagues have devised one-question screens that may help determine whether a patient will be able to understand medical information. A doctor could ask, “How confident are you in filling out medical forms by yourself?” or “How often do you have someone help you read hospital materials?” A 2012 review of studies that compared those single questions to REALM and TOFHLA found that the much simpler tests often sufficed to determine health literacy. For example, a patient who says he “always” gets help reading hospital materials (rather than “often,” “sometimes,” “occasionally” or “never”) tends to fit the TOFHLA definition of inadequate health literacy.
Yet not everyone believes patients should be screened at all. “It’s extremely controversial,” says Dean Schillinger, a researcher at the University of California, San Francisco and a co-author of the 2005 study that found physicians overestimated the health literacy of patients even when they knew a significant proportion of their patients had limited literacy. “There’s a reluctance to stigmatize patients as having limited literacy skills—a scarlet letter effect.” Rather than try to determine how literate a patient may be, he prefers to put the onus on doctors to communicate clearly at all times, as if every patient had limited literacy. “Straightforward communication is better for everyone,” he says. Then, if patients use technical terms, doctors can ratchet up the complexity of an explanation.
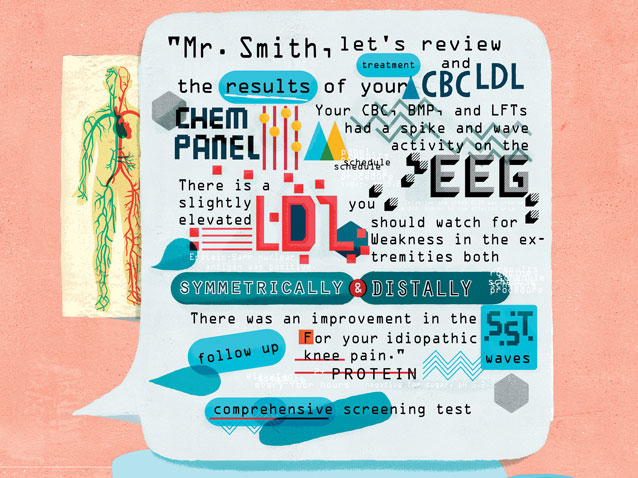
Research does suggest that the communication skills of physicians and other caregivers have room for improvement. In a 2007 study of diabetics, for example, researchers audiotaped 74 doctor-patient encounters and found that eight out of 10 were characterized by medical jargon the doctors didn’t explain, with an average of four unclarified terms per visit. When patients in the study were later asked the meaning of various diabetes terms, their comprehension tended to be low, even though many had indicated that they had been able to follow their doctors’ explanations.
Schillinger advocates eliminating all jargon, using pictures, and applying the “teach-back” method. “Doctors say, ‘Oh, I do that,’” says Schillinger. “They ask, ‘Do you understand? Have I been clear?’ But the teach-back method is, ‘So, we’ve talked a lot about your fibroids and the different treatment methods we have. When you go home and your husband asks what the doctor told you, what will you say? Because I want to make sure I’ve explained it to you clearly.’”
Technological solutions might also help improve patient literacy—or they could make things worse. Increasingly, patients are being directed to online portals to get access to lab results and medical records and to help manage their own care, and anyone who isn’t comfortable using a computer may be at a disadvantage. Still, according to a 2009 study, some patients with low health literacy would prefer to “interact” with a well-designed computer program than speak with a clinician, who may be condescending or explain things poorly.
One interesting technological innovation is the “embodied conversational agent”—a character on a computer screen that looks at users, gestures to them and utilizes programmed “best practices” for health education. Research suggests patients may learn more from such characters than from humans and may tend to ask them more questions. It also helps that patients can spend as much time as they want with these virtual teachers.
IN 2004, MICHAEL WOLF, professor of medicine and learning sciences at Northwestern University’s Feinberg School of Medicine, established the Health Literacy and Learning Program (HeLP). The program may be the only one of its kind in the United States to “link the fields of medicine and education in order to improve how health systems educate patients and families on their health.” Researchers at HeLP investigate ways to improve health literacy, and one of the biggest lessons so far, says Wolf, is that the problems transcend individual doctors or patients.
“The level of difficulty of any health care task is determined by the health system that created the task,” says Wolf. “So, you can’t look at individuals without understanding the context of the system in which they’re situated.” A study published by Wolf’s group in 2011, in which subjects were given hypothetical regimens of seven drugs and asked to determine when they would take each drug, found that the subjects significantly overcomplicated their daily schedules. Absent additional guidance, many created a schedule to take medicine seven times a day when it could have been taken four or fewer times a day, and maintaining such a schedule may be particularly difficult for those with low health literacy. And in the real world, the instructions patients receive can also be overly complex. In one practice that Wolf’s team examined, clinicians had 53 ways to say “Take one tablet a day.”
Wolf’s group has been addressing this prescription problem by coordinating clinician and pharmacy efforts through electronic health records. They found that a simple solution, such as having pharmacists divide medications into morning, noon, evening and bedtime blocks, can significantly ease the burden on patients.
In another effort to approach health literacy issues at an overarching level, Dean Schillinger recently co-wrote a paper for the Institute of Medicine entitled “Ten Attributes of Health Literate Health Care Organizations.” He and several other authors identified steps that they believe could improve health literacy. Among them are organizational leadership that “makes literacy integral to [an institution’s] mission, structure, and operations” and creating a system of care that “meets the needs of populations with a range of health literacy skills while avoiding stigmatization.” Also important, according to the IOM paper, is communicating clearly to patients “what health plans cover and what individuals will have to pay for services.” At this point, Schillinger says, “we’re far away from doing any of those things. But if we can fix the communication problems in health care, we won’t solve everything, but we will make a dent.”
AN EARLIER IOM PAPER, in 2004, called for a concerted effort to publicize and address the issues of health literacy, and in 2010, the U.S. Department of Health and Human Services issued an action plan that ranges from improving health and science curricula in schools to encouraging changes in the health care system to promote informed decision making. Yet such efforts come at a time when patients are being asked to take more and more responsibility for the details of their medical care—and when, as part of a shift toward shared decision making, many patients indeed want to help direct their own care in a much more active way. Adequate health literacy is a prerequisite for that larger role, and physicians who attempt to help patients weigh the pros and cons of treatment options may find their efforts hindered by patients’ inability to understand complex trade-offs.
In other cases, patients don’t seem interested in learning more or in taking responsibility for helping make decisions about their care, preferring just to go along with their doctor’s recommendations. “There could be a whole host of reasons why people are not engaged in their care decisions, such as challenges in navigating the health care system, a perceived lack of empowerment, or personal reasons,” says Sarah Collins, a nurse informatician at Partners HealthCare in Boston. “But if we can determine that a lack of literacy is why they don’t want to engage, we could intervene.”
Such interventions take time, and considering how little of that precious commodity doctors tend to have with patients, addressing health literacy issues may seem like just one more demand on an already overburdened provider community. Yet Schillinger contends that much of what’s needed is something caregivers can learn to provide almost without thinking about it. “When I try to teach my teenager American history, he doesn’t want to hear it,” he says. “But if I engage him in a discussion about what’s important to him, I might be more effective. We just need to do some creative pedagogy, to actually have a conversation. I take care of the sickest, most socially vulnerable patients who don’t speak English, have alternative health beliefs and have low health literacy. Yet only a handful defer decision making to me. I have never met a person who does not want to learn about her own body. You need to make sure that you’ve given the person the opportunity to engage.”
Dossier
“Health Literacy and 30-Day Postdischarge Hospital Utilization,” by Suzanne E. Mitchell et al., Journal of Health Communication, October 2012. Details of the finding that patients with low health literacy are significantly more likely to be readmitted to the emergency department within 30 days of discharge than people with adequate health literacy.
“Health Literacy Screening Instruments for eHealth Applications: A Systematic Review,” by Sarah A. Collins et al., Journal of Biomedical Informatics, June 2012. This review of 11 health literacy screens found that asking a single question (such as “How often do you have someone help you read hospital materials?”) can reliably pinpoint people who need additional help understanding the medical system.
“Babel Babble: Physicians’ Use of Unclarified Medical Jargon with Patients,” by Cesar M. Castro et al., American Journal of Health Behavior, September-October 2007. Reviewing audiotaped physician interactions with patients with low health literacy, researchers found that patients mostly did not understand physicians’ instructions, even when physicians were sure they did.
Stay on the frontiers of medicine