Published On July 23, 2008
WHEN JAY CROSS READ ABOUT THE NEW service from startup genomic-testing firm 23andMe, part of the appeal was academic. Cross, a 63-year-old business consultant, is naturally curious, and he was drawn to the idea of participating in cutting-edge science. But he was even more interested in what he might glean from his DNA about his personal health struggles. At 44, Cross had quit smoking and started running, only to suffer a heart attack shortly thereafter. Another followed a few years later. Cross, who also battled depression and attention deficit disorder, started to wonder, “Am I genetically predisposed to all this, or have I just been a bad boy?”
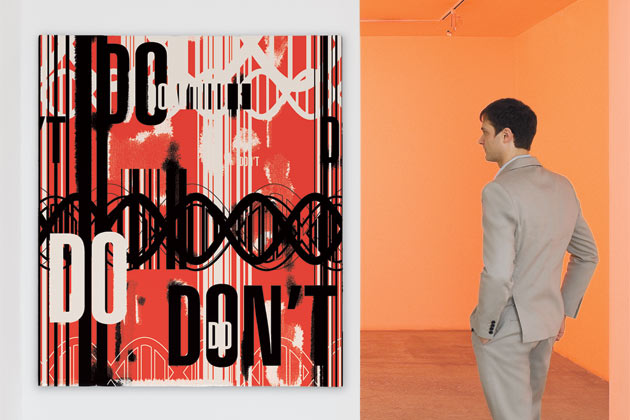
For $999, 23andMe offered insights into this fundamental question of nature vs. nurture. After making his payment, Cross deposited some saliva in a tube and mailed it off to the firm’s Silicon Valley headquarters. Researchers at the company, which was launched in autumn 2007 with the slogan “Genetics just got personal,” scanned the DNA sample and posted his results on password-protected Web pages.
With millions of genetic variations that differentiate one person from the next, the human genome is astonishingly revealing: Anyone who has wondered why he has green eyes will find the answer right there, in the genes, and the presence of certain genetic variations may partly explain why he is particularly adept at hitting a fastball. But 23andMe also offers a peek over the horizon, showing genetic predispositions to any number of conditions, from cancer to diabetes and arthritis.
Other new arrivals to the fledgling genomic-testing business include Navigenics and deCODEme. Many feature quirky applications; ScientificMatch, for example, offers a dating service, sorting potential mates based partly on genes associated with the immune system, theoretically increasing the chances that a couple will have offspring with robust immunity. Sciona promises a customized diet and lifestyle regimen based on an analysis of 24 genes. Almost anything seems possible, and genetic testing has become an estimated $730 million industry that is expected to grow 20% annually.
But 23andMe, named for the number of paired chromosomes that make up each genome, is the splashiest new DNA vendor. When Jay Cross logged on to the 23andMe Website to see his results, he learned that his extended family originated some 45,000 years ago on the Arabian Peninsula. Perusing his “Gene Journal,” Cross found other similarly arcane factoids, including his propensity for restless leg syndrome and his earwax type. But he was stunned to learn that, genetically speaking, he was 20% less likely than the average person to have a heart attack. He wasn’t sure whether it meant his lifestyle had brought on his heart problems or he had just been unlucky. Nor did he have a clear idea of what lay ahead. “I didn’t need to pay $1,000,” he says, “to find out about my earwax.”
Cross was learning what geneticists already know: that though genomic science holds great potential to tell us who we are and what maladies we may get, such tests are now of limited value. The startup firms’ decision to market highly complex tests directly to the public, often without any kind of expert on hand to interpret the results, has sparked considerable controversy and even the threat of legal intervention by state regulators. There’s a fear that people will take the results too literally and request batteries of unnecessary tests—or, perhaps worse, be lulled into a false sense of security.
The new firms argue that they are providing a service that has educational value and will inevitably become useful, as scientists move toward linking genes more clearly with cancer and other diseases. Linda Avey, co-founder of 23andMe, acknowledges that genomic-testing providers might not yet be able to deliver a great deal of useful information about illnesses people commonly worry about, but she expects that to change soon. “Our message to customers is, this is ongoing,” Avey says. Every time scientists achieve a breakthrough in a gene-association study, 23andMe adds that information to its database, expanding the information available to its customers. “It’s early, but more information will come out and we’ll get better and better about reporting it back to people,” Avey says.
But that begs the question of what happens in the meantime. Should someone—the government, the medical community—try to rein in these firms or discourage patients from putting stock in mail-order diagnoses? Or are people entitled to search the contents of their own DNA, whether what they learn is good for them or not?
HUMANS HAVE SOME 6 BILLION BITS of genetic code in their DNA. Among these are about 20 million gene variations called single nucleotide polymorphisms (SNPs, pronounced snips). SNPs are chiefly responsible for making one human being different from all others. In the 1990s, scientists began looking for groups of people with the same SNPs who also have, say, colon cancer. Find enough who have both the same SNP pattern and colon cancer, and they might identify a genetic signpost for the disease.
Some of these “association” studies have led to breakthroughs. Already, thousands of women each year take tests for mutations in BRCA1 and BRCA2, two genes associated with a highly hereditary form of breast cancer. Researchers have also pinpointed a few monogenic conditions, in which a single genetic variation is directly connected to a particular ailment, such as Huntington’s disease. If you have the Huntington’s SNP, you’ll almost certainly contract the disease.
But it wasn’t until a few years ago that researchers began to unlock the vaults of information stored in our genes. In 2003 scientists completed the Human Genome Project, which mapped our common genomic sequence, determining the order of four component chemicals in each of our DNA’s 3 billion base pairs and identifying all of our approximately 20,000 genes. Two years later they finished the first phase of the HapMap Project, an effort to catalogue common patterns of SNPs that initially pinpointed 1 million variations. Phase 2, completed in October 2007, added 2 million more SNPs. Not surprisingly, the connections between genes and disease are turning out to be extremely complex, with the interplay between genes and prevalent ailments still undeciphered. Diet, lifestyle, environmental factors and stress also come into play, and the presence of certain SNPs, as revealed by some of today’s genomic tests, is just one of many possible contributing factors.
Amid such uncertainty, David Altshuler, a geneticist and physician at the Massachusetts General Hospital and Harvard Medical School, has turned down offers from DNA vendors to scan his genome. “Right now, there isn’t enough known to make the offerings of these companies clinically useful,” Altshuler says.
Consider type 2 diabetes. If Altshuler’s patients want to gauge their chances of developing the disease, they could be tested for the TCF7L2 gene, a mutation carried by more than a third of the population that increases the odds of the disease’s onset by more than 45%. But environmental factors and diet also play a huge role (obese people are much more likely to become diabetic), and many unmapped genes might be even more closely associated with the disease. Today, Altshuler says, reviewing a patient’s family history reveals more than a test showing the presence of TCF7L2—“by a long shot.”
The science, in other words, currently lags the hype. “If there’s one take-home message in what scientists have learned about genomics during the past 10 years, it’s that this is a lot more complex than we ever thought,” says Jesse Reynolds, director of biotechnology accountability at the Center for Genetics and Society in Oakland.
Some think this need not be a deterrent. Elissa Levin, director of genetic counseling at Navigenics, says that customers have shown an ability to grasp that genetics are just one part of the equation. “There’s a shift away from the idea that genes are our destiny,” she says. “What I keep hearing is that our service is really a heads-up. People actually feel empowered.”
What’s more, there continue to be breakthroughs in linking genes to disease. In a prostate cancer study published last January in The New England Journal of Medicine, researchers at Wake Forest University School of Medicine in Winston-Salem, N.C., and other institutions reported that a grouping of common, minor variations in five areas of DNA can go far in forecasting the risk of getting the disease. In a study of nearly 5,000 men, the researchers found that 90% had one or more of the SNPs, and more than half had two or more. The cancer risk grew as the number of variants increased. Those who had at least four of the variants were five times more likely to get prostate cancer than those who had none. Add in a family history of prostate cancer, and risk of the disease skyrocketed to nine times that of men with no genetic risk factors.
On the face of it, these study results seem to underscore the promise of genetic testing. But the blood test that the Wake Forest scientists developed cannot predict which men will get aggressive cancers, and merely knowing you have a heightened risk of prostate cancer could lead to excessive screening, unnecessary surgery and complications.
The Wake Forest scientists have formed a company, Proactive Genomics, hoping to market their Focus5 blood or saliva test this summer. But even though the science behind the test is remarkable, questions about how the results may be used also underscore the unintended consequences that may come with widespread genetic testing. What will a patient do if he learns he has 10 times the normal risk of prostate cancer? And what happens when deCODEme customers see they have a high risk of, say, heart disease? Should they go on a diet? Start exercising more? See a doctor?
WITH MOST MAIL-ORDER TESTS, consumers are left to interpret and perhaps act on the information they receive. Navigenics, deCODEme and DNA Direct offer customers access to counselors who can interpret the results, but many others only provide Internet links to studies showing the underlying research. And although most companies include caveats regarding any connections between their services and medical diagnoses, that may seem disingenuous when the information consumers receive apparently has a crucial connection to their current and future health. “No matter how often these Websites’ warnings are repeated, individuals may have a difficult time accepting them,” says Greg Feero, chief of the genomic-health-care branch of the National Human Genome Research Institute.
“Scanning someone’s genome is a personalized service,” says Jesse Reynolds of the Center for Genetics and Society. “But with most of these tests, it’s done in the absence of actually communicating with anyone.” Reynolds’s main worry isn’t that people will begin flooding doctors’ offices with deCODEme printouts. Only about 800 physicians in the United States have significant training in genetics, leaving the rest ill equipped to interpret the results. He actually fears the opposite will happen: A customer of a genome-testing outfit who learns he has only a modest risk of heart disease could presume he’s in the clear, even if his lifestyle leaves much to be desired. “I’m concerned that people could underreact,” Reynolds says.
FOR NOW, REGULATION OF GENOMIC-TESTING services is minimal, and that leaves consumers with few assurances about the accuracy or value of the information they’re buying. “There’s a basic lack of oversight, and that makes it difficult to determine which tests are ready for prime time,” says Gail Javitt, law and policy director of the Genetics & Public Policy Center at Johns Hopkins University in Baltimore. “There are very few barriers to market entry for these tests.”
But state regulators, increasingly, are taking notice. In September 2007, for example, testing service Myriad Genetics launched an advertising blitz promoting BRACAnalysis, its test (which must be ordered by a physician) for identifying the BRCA1 and BRCA2 mutations. That sparked an investigation by the Connecticut attorney general’s office into the truthfulness of the ads (Myriad is cooperating fully in the investigation).
Such investigations have only increased in frequency. Last November, New York’s Department of Health sent letters threatening fines and jail to 26 online gene-testing companies, saying they are violating state law by offering services without the involvement of “a qualified person, such as a physician licensed to practice medicine in this state or other authorized ordering source….” Many have submitted business plans for the state’s review and are cooperating fully. And in June, the state of California sent letters to 13 genetics firms requiring proof that they are complying with state laws that require, among other things, that physicians are ordering the tests on behalf of their patients.
“Without the proper guidance, it’s difficult for people to figure out whether it’s appropriate to spend money for that kind of test,” says Erin Tracy, a physician at the MGH who wrote an article on the subject in the journal Obstetrics & Gynecology.
But there’s a fine line between protecting consumers from uninterpreted information and preventing them from learning possibly crucial facts about their health. Altshuler, the MGH physician and geneticist, doesn’t buy the idea that simply offering up genetic data is harmless at worst and empowering at best. “If a test leads to further tests, and those further tests have side effects—they involve a biopsy, for example—they can lead to anxiety or suffering,” he says. He expects that once the current fad for testing fades, firms that don’t offer anything of value won’t survive. “If recreational users can’t explain to their friends why it’s worth $1,000, it won’t go anywhere,” he says.
For now, 23andMe’s Avey suggests, the firm’s most important role might involve connecting consumers with similar traits (imagine a Facebook page for, say, cystic fibrosis patients) and perhaps sparking grassroots research efforts. Researchers often are stymied by a lack of study participants. But if more people learn through genome scans that they’re susceptible to a particular disease, they may be more likely to sign up.
Eventually, the kind of information provided by testing firms will play an important role in modern medicine, with more and more disease-causing SNPs identified and the impact of environmental and behavioral factors sorted out. And it’s that promise that keeps Jay Cross, the two-time heart attack victim, hanging in there with his 23andMe account, through which he continues to get updates at no additional cost. He thinks that if he’s patient, the science will catch up to the hype that lured him in. “I thought it was a lot closer to being a bottle of wine that was ready to drink,” he says of his DNA scan. “But essentially what I bought was a Bordeaux future.”
Dossier
“Are Doctors Prepared for Direct-to-Consumer Advertising of Genetic Tests?” by Erin Tracy, Obstetrics & Gynecology, December 2007. Clear-minded and succinctly worded, Tracy’s analysis cites both anecdotal evidence and numerous studies to suggest that DNA vendors are taking advantage of consumers—and to argue that genetic testing needs to be reined in.
“Breakthrough of the Year: Human Genetic Variation,” by Elizabeth Pennisi, Science, December 2007. With this opus in praise of new technologies able to sequence DNA and assess variations in genomes, Pennisi argues compellingly that the best is yet to come.
A Short Guide to the Human Genome, by Stewart Scherer (Cold Spring Harbor Laboratory Press, 2008).Laid out in an easily digestible question-and-answer format, this essential primer details the underlying science in the direct-to-consumer genetic testing debate.
Stay on the frontiers of medicine
Related Stories
- Your Genes Have Been Scanned. Now What?
New studies aim to determine what consumers do—or don’t do—after they’ve had a mail-order genome test.