Published On May 20, 2021
IN SPRING 2020, WHEN the COVID-19 pandemic was first raging through sub-Saharan Africa, Hassan Nsabimana was among countless truck drivers who continued to work transporting essential cargo to Rwanda from neighboring countries. In a phone conversation last May from Tanzania, Nsabimana told his eldest son, Faycal Hassan Tuyishime, that he wasn’t feeling well and was heading home. “In his voice, you could tell he was critically ill,” Tuyishime says.
It was their last conversation. Nsabimana, 65, was tested for the virus at a border checkpoint, then rushed by ambulance to Rwanda’s main COVID-19 treatment center in Kigali, the capital. By then, he was having trouble breathing and was put on a ventilator in intensive care. He died two days later and was the country’s first fatality linked to the virus. His death was widely reported in Rwanda—in part because at the time, COVID-19 was still relatively rare in the nation of some 13 million people. In late May, the country had fewer than 400 confirmed cases.
That Rwanda has continued to fare relatively well by the grim statistical measures used to gauge the impact of COVID-19 most likely came as a surprise to much of the global public health community. Most of Africa, which had been ravaged by AIDS, Ebola and other contagions, was thought to be ill prepared for a pandemic. In the 2019 Global Health Security Index, which assessed 195 nations’ preparations for the kind of global outbreak that would begin a year later, the United States ranked highest, followed closely by the United Kingdom and other developed countries. China ranked 51st, and most African countries were at the bottom.
Rwanda is one of the world’s poorest countries, with annual per capita income, adjusted for cost of living, of just $2,000 in 2020. A high population density of 525 people per square kilometer—more than 14 times the density of the United States—also seemed likely to encourage the spread of an extremely infectious disease.
Denmark, in contrast, ranks among the wealthiest nations, with a 2019 per capita annual income of $65,147. Its pandemic preparedness ranked eighth in the Global Health Security Index, just behind Sweden and ahead of South Korea. The population in 2021 was just 5.8 million, and there were only 135 people per square kilometer. So Denmark’s relative success in confronting the pandemic is perhaps less surprising. At the end of the pandemic’s first year, the country had seen a much heavier toll than Rwanda, with 2,385 deaths compared with the African country’s 273. But the impact of the disease in Denmark has been only about a third as high as in Switzerland, for example, a slightly more populous European country of comparable geographic size.
The pandemic responses in both Denmark and Rwanda have been vastly more effective than those of the United States and many other much larger global powers. While very different from each other, the two nations have both benefited from having trusted, government-run health care systems, consistent public health messaging and smart use of the technology available to them. Having the courage to tell the truth about COVID-19 and impose often unpopular restrictions has also played a central role in their still unfolding strategies. But it’s in the finer details of what they’ve done that there are lessons, perhaps, for other health care systems.

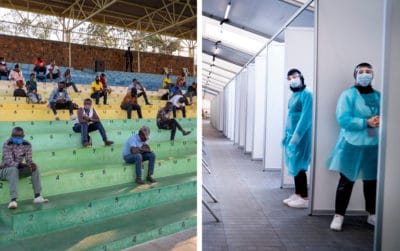
Source: Left: Bo Amstrup/Getty Images; Right: Xinhua News Agency/Getty Images
In much of Africa, medical resources are limited, health systems are fragile and even before the pandemic, half of the continent’s deaths were caused by infectious diseases. And in Rwanda, mathematical models created in January to predict the likely consequences of COVID-19 showed a health care system almost sure to be overwhelmed, says Menelas Nkeshimana, a physician at the University of Kigali Hospital and vice chair of the Rwanda Medical Association. The nation’s best chance, Nkeshimana says, was to keep the new disease from becoming widespread. “Preparedness was vital to us,” he says.
So in January, many weeks before the first coronavirus case was detected, the government formed a joint task force for COVID-19. Beyond the fairly standard recommendations it made, such as canceling flights from China and giving COVID-19 tests to all travelers entering the country, the task force also deployed tools that had helped in preventing and treating HIV and Ebola—mobile phone apps, GPS, artificial intelligence and electronic tools for conducting home-based monitoring.
“For the most part, African leadership took the pandemic seriously at the right time,” says Rahul Joseph, a program manager at Surgo Ventures, a nonprofit in Washington, D.C., whose Africa COVID-19 Community Vulnerability Index (CCVI) assesses health, economic and social impacts of the pandemic. Rwanda ranks among the least vulnerable nations in the Surgo index—with a scale of 0.003 CCVI.
Rwanda’s decentralized health care system was built from the ground up after the 1994 genocide that left the country in ruins. Although there is only about one physician per 10,000 people, the system provides universal coverage while granting considerable autonomy to community health workers spread across the country. The system is also extremely popular. In a pre-pandemic study from the Wellcome Trust in 2019, 97% of Rwandans expressed confidence in their health sector—a higher approval rating than anywhere else in the world—which proved to be a powerful benefit in facing down a global viral onslaught. “People know the system is not against them and that public health guidance is based on science and not politically motivated,” says Agnes Binagwaho, vice chancellor of the University of Global Health Equity in Rwanda, a former health minister and a key architect of the modernized system. “If the health minister says something is good for you, people will do it because of trust.”
As the pandemic found its way into Africa, Rwanda mounted a public awareness campaign to inform Rwandans about how the new coronavirus was transmitted and urging them to take measures to slow its spread. Later, everyone was required to wear face masks in public and encouraged to submit to testing and contact tracing. These messages were disseminated on social media platforms, radio, television and newspapers and broadcast from vans driving through neighborhoods.
On March 14, Rwanda announced its first confirmed COVID-19 case. A week later, the government instituted a national stay-at-home order, closed borders to all but essential goods and cargo and suspended commercial air travel. It was one of the first lockdowns in Africa.
From the beginning, testing was widespread, and health authorities didn’t wait for people to come to them. Instead, medics in protective gear stopped people randomly on the streets to offer tests, then sent samples to labs that in many cases repurposed equipment designed to detect HIV infection. Researchers at the University of Rwanda devised a system for pool testing, which enabled two dozen tests to be processed in one batch. If infection was detected, technicians went back and tested each sample. Pool testing proved faster and cheaper, and by August, Rwanda was conducting 10,000 tests a day.
As the outbreak escalated, a small army of newly trained contact tracers was deployed, and anyone who had come into contact with an infected person was called or visited and had to quarantine until a COVID-19 test could be administered. At the COVID-19 task force command post, computer dashboards displayed real-time data pinpointing geographic areas where cases were spiking.
Other technology also boosted Rwanda’s response. Drones, already used to deliver blood and medical supplies to remote regions, now were deployed to distribute COVID-19 tests, personal protective equipment and other pandemic-related items. Drones have also been used by police for surveillance, to spot large groups gathered in violation of government edicts.
Then there were the robots. On May 19, at the COVID-19 Treatment Centre in Kan-yinya, Health Ministry officials introduced five human-sized robots manufactured by a Belgian company that were designed to reduce human interactions and the risk of viral transmission. They could screen more than 50 people per minute for common virus symptoms—fevers, dry coughs—as well as deliver food and medication to patient rooms. One robot was deployed at Kigali International Airport to screen incoming passengers, and the others were sent to treatment centers and out onto the streets, where they could detect people without masks or who were wearing them incorrectly and instruct them in proper usage. At treatment centers in Gatenga and Kanyinya, the availability of the robots has cut the exposure of human providers to infected patients almost in half.
All of these efforts seemed to pay off, and by late spring, with case counts stable or falling, the government began easing the lockdown in phases. There was still a nightly curfew, but by early June, the country was open for domestic travel and tourists from outside the country were allowed in. Then, when infection surges were detected—at the borders, in markets, in prisons and elsewhere—more restrictive measures were put back in place. “Localized testing and lockdowns are two measures that Rwanda has done well,” Joseph says.
In late October, the World Health Organization applauded Rwanda “for instituting a strong system” that enabled the country to “effectively confront” the COVID-19 pandemic. And in January 2021, Rwanda’s response ranked sixth globally and first among countries in Africa in the COVID-19 Performance Index compiled by the Lowy Institute, an Australian think tank.
Still, human rights groups have criticized the authoritarian government’s tactics in enforcing public health measures. Not wearing masks or breaching social distancing rules can result in fines, or jail for multiple offenses, and anyone who tests positive for the virus but still mingles with the public could be subject to a two-year imprisonment. Citizens detained by security forces for violating curfews have reportedly been forced to spend the night in a stadium listening to public health broadcasts blaring from loudspeakers.
Source: Left: STR/Getty Images; Right: Liselotte Sabroe/Getty Images
ONE OF DENMARK’S MAIN advantages in confronting the pandemic is the country’s social cohesion. According to the European Values Study, which maps attitudes, beliefs and behaviors in European countries, Danes have the continent’s highest level of social trust in one another. They also believe in Denmark’s government-run health care system, which is free for everyone and is considered one of the best in the world. There’s high regard for science, and some Danish habits, such as not typically hugging in greeting, have amounted to a kind of natural social distancing.
But perhaps Denmark’s biggest edge comes from being one of the most digitized countries in the world. Every citizen has a 10-digit personal identification number linked to a central national registry, and that electronic infrastructure proved crucial in supporting the country’s COVID-19 testing and detection strategies and enabling detailed epidemiological research throughout the pandemic.
As with other countries, Denmark also closed its borders, shuttered schools and other public institutions and banned gatherings of more than 10 people. But the government didn’t restrict travel inside the country or issue curfews or stay-at-home orders, and there was no government-enforced contact tracing. “While Danes are very trusting and law obeying, people are very much against unnecessary supervision by the state,” says Trine Mogensen, a physician and researcher at Århus University Hospital and co-author of an online medical journal article that analyzed the country’s pandemic response.
A central pillar of Denmark’s containment strategy has been free COVID-19 testing available to everyone, and whenever someone tested positive for COVID-19, that anonymized result was recorded in the national system, with information about where and when it occurred. “We can detect what COVID transmission patterns look like in real time,” says Jens Lundgren, professor of infectious disease at the University of Copenhagen and Rigshospitalet.
Users of mobile apps also contributed to the well of data available to the government and to medical researchers. Smittestop, which means “halt infection,” notifies people when they come near someone infected with the virus and was downloaded by 12% of Danes in the first two weeks it was available. Moreover, the Danish population has long been accustomed to digital communications from government authorities, and in spring 2020, a text alert to every mobile user in the country announced a new fine for failing to observe social distancing guidelines. When the Danish Patient Safety Authority announced it was setting up a secure email system to allow the anonymous reporting of anyone suspected of having COVID-19, however, public backlash led to a quick reversal.
The first wave of infections peaked the first week of April, when 535 patients in Denmark were hospitalized and 146 were in intensive care. The government then began a phased removal of restrictions. As a small economy dependent on foreign trade, the nation had taken a big economic hit when it shut down, and reopening was a political priority. Denmark was the first in the European Union to reopen primary schools, day care centers and some small businesses, and a month later, retailers, restaurants and secondary schools also opened and cultural activities were allowed to resume. Limits on public gatherings were eased, and border crossings resumed.
During the summer, as infection numbers continued to fall, health authorities settled on an approach they called “the green curve.” They would take actions to suppress the pandemic as needed to minimize the strain on hospital capacity but would otherwise let infection levels peak and decline naturally as immunity in the overall population increased. “We looked to the testing infrastructure to manage the fluctuations,” Lundgren says.
That strategy worked during the summer months, when several small local outbreaks were identified and contained. But in early August, infections surged in Århus, Denmark’s second-largest city. Hundreds of new infections were detected, particularly within the Somali community, with contact tracing linking many of those cases to a large funeral. Testing through the fall, in Århus and much of the rest of the country, revealed a second wave of the pandemic.
During that second wave, the Danish tracking system showed a surprising source of new infections. It was discovered that mink could become ill with COVID-19 and could spread the virus to humans. When mink-linked human infections climbed to more than 200 cases by November, health authorities quarantined workers and conducted extensive testing of more than 280,000 people. In late November, the government dictated that all of the mink on 289 farms where infections had been documented, as well as those on other nearby farms, would be killed. That added up to 17 million animals.
Lundgren believes mink-sourced infections contributed to the fall surge of the disease. But a far larger factor behind Denmark’s second wave was public complacency, he says: “People just stopped paying attention to advice.” In early December, with new infections running at about 3,000 a day, partial lockdowns were rolled out in areas covering about two-thirds of the country.
But this time, hospitalized COVID-19 patients benefited from a growing arsenal of treatments. Danish physicians and patients continue to participate in many international trials of experimental drugs and vaccines. In addition, data from widespread testing in Denmark—more than 10 million tests of 4 million people, covering 70% of the population—facilitated the world’s first large-scale study of COVID-19 reinfection rates. The findings confirmed that most people who have had COVID-19 are protected from catching it again for at least six months, although older patients are more prone to reinfection.
DENMARK HAS BEEN A pioneer in tracking COVID-19 mutations through genomic sequencing of positive tests, and concerns about virus variants, including the B.1.1.7 variant first detected in the U.K., have risen. Moreover, a renewed lockdown implemented at the end of 2020 was only starting to be eased four months into the new year. But the rollout of COVID-19 vaccinations was proceeding, and the government hoped to have the entire population inoculated by July.
Rwanda, experiencing its own wave of infections in early 2021, imposed another lockdown in the capital, banned movement among regional districts and lengthened curfew hours. But as numbers of new cases and deaths fell by half, some restrictions were eased. By early April, just under 400,000 vaccine doses had arrived, and the government said it hoped to provide shots to about a third of Rwanda’s population by the end of the year, with the remaining two-thirds getting vaccinated in 2022.
In both of these countries, like everywhere else in the world, the battle against COVID-19 has not quite ended. Yet even now, as the United States, under a new administration, looks at home and abroad for insights into what did and didn’t work in combating this pandemic—and how to better prepare for future viral onslaughts—the experiences of Rwanda and Denmark may offer strategies disproportionate to their small geographic footprints.
Dossier
“Rwanda’s Secret Weapon Against COVID-19: Trust,” by Eli Cahan, The BMJ, December 2020. In this interview, Agnes Binagwaho, an architect of Rwanda’s health system, describes how the country managed the first wave of the virus despite lacking certain resources.
“The COVID-19 Pandemic in Denmark: Big Lessons From a Small Country,” by David Olagnier and Trine Mogensen, Cytokine Growth Factor Review, June 2020. Researchers examine how Denmark weathered the COVID-19 crisis with a relatively low rate of infection.
Lowy Institute COVID Performance Index. This interactive website measures how certain factors are impacting the COVID-19 response in more than 100 countries.
Stay on the frontiers of medicine
Related Stories
- Chapter 1: In the Path of the Pandemic
A novel coronavirus would come to affect every ward, clinician, researcher and patient at Massachusetts General Hospital.
- Chapter 2: The Virtues of Necessity
As the first COVID-19 patients arrived, pressure mounted to discover how the disease worked and how it could be beaten back.
- Chapter 3: The Fight That Lies Ahead
When the caseload began to ease, clinicians came to grips with the new normal as researchers set their sights on ending the pandemic for good.