Published On November 20, 2021
Frustrated by his experiences with statins, “Noah” let his doctor enroll him in a clinical trial. He knew that he needed to lower his cholesterol, but all three drugs he had tried seemed to cause debilitating muscle pain—a common reaction to statins that has puzzled many physicians because the original studies testing the drugs for safety and efficacy showed that such outcomes should be rare.
The trial Noah’s physician proposed was unusual. The gold standard for knowledge in medicine has been, for many decades, the randomized control trial (RCT), which typically involves a large number of subjects randomized into either experimental or control arms, with the results assessed to see which alternative offers the better benefit. If a large number of patients do well with the new treatment, it’s considered a success. If only a few patients benefit, the control is considered the better course. But the trial that Noah would undergo had only one patient—Noah himself—and success would be gauged on his reaction alone.
For the next year, Noah would act as both the control and the experimental arms of his own study. He would take a statin for four months out of the year (not necessarily consecutive), four months of a placebo and four months of no medication. Each day he would record any side effects. While he did this, 48 other patients were enrolled in similar, stand-alone studies. The findings of each trial would be personal. For instance, two participants found that during their months on statins they experienced disabling side effects, which went away when they took the placebo or no medication. “There was nothing in these patients’ histories to indicate they would have trouble taking a statin,” says James Howard, a cardiologist at Imperial College London and the trial’s investigator.
But for Noah, something more surprising happened. “He nearly left the trial after the first few months because he felt so dreadful,” says Howard. “But that was when he was on placebo. The fourth month, when he was actually on the statin, he felt fine.” Reviewing the final data, Noah was “gobsmacked” that his response to statins appeared to be more psychological than physical. The evidence argued that pain stemmed from the “nocebo effect”—because he expected to feel terrible taking statins, he did. It convinced him to go back on the medication, and in the four years since, his muscle pain hasn’t returned.
Noah’s trial had an N of 1—in clinical research, N denotes a study’s number of subjects—and now the N-of-1 model for this kind of personalized scrutiny is experiencing something of a renaissance. At first glance, an N-of-1 trial resembles any medical encounter in which a patient visits a physician to find treatment that works. But the average patient journey falls far short of the rigor of clinical research. “Physicians do a considerable amount of trial-and-error prescribing, which can be very flawed,” says Heather Kaplan, associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center. “We start patients on a new drug and ask how they feel. If they say OK, they may stay on the drug for years, even though the improvement they describe may not actually be directly related to the new drug.”
The N-of-1 trial, in contrast, offers a framework for gathering information “systematically and rigorously,” Kaplan says. She is conducting N-of-1 trials on children with inflammatory bowel disease, with the goal of discovering, with confidence, which participants can control the disease through diet. For kids who respond to a dietary intervention, the trial investigates what specific diet works best.

Although huge RCTs can predict treatments that benefit the average patient, “I’ve never met an average patient,” says neurologist Steven Arnold, managing director of the Interdisciplinary Brain Center at Massachusetts General Hospital. The success of any treatment is influenced by genetics, the patient’s progression in a disease, other illnesses the patient may have, and environmental and lifestyle factors such as levels of exercise and stress. Typical parallel-group RCT trial results may not account for these, Arnold says, and it falls to the physician to map the best treatment in a personalized way.
The N of 1 is a tall order, however, and such trials have historically required more effort than most physicians can give. That may be changing, however, says Ian Kronish, associate professor of medicine and co-director of the Hypertension Center at Columbia University Irving Medical Center. Digital medical devices and smartphones can now seamlessly track and transmit data, enabling doctors and patients to create N-of-1 trials to shape joint decisions, and genetic analysis of individual patients has become more accessible. For conditions that are hard to measure objectively, such as cognitive decline, N-of-1 trials may offer new pathways to improvement. And for patients who fall outside the treatment norm, these studies are a way to find the most effective treatment. Patients may serve not only as guinea pigs but as research architects and investigators.
The legacy of N-of-1 trials in mainstream medicine dates to the 1980s and the work of physician Gordon Guyatt. In a 1986 article in The New England Journal of Medicine, in which the term “N of 1” first appears, Guyatt and his colleagues at McMaster University in Ontario, Canada, note the physician’s “paradox” of having to use large RCTs to guide individual treatment when, in those trials, “experimental therapy almost never benefits every patient randomly assigned to it, and it usually harms at least some … [and] even when a relevant randomized trial has generated a negative result, at least some patients will appear to have benefited.”
The paper described a trial designed to test drugs on a single patient, a 65-year-old with uncontrolled asthma. “We found out the therapy we were giving the patient was killing him,” recalls Guyatt, now distinguished professor of health research methods, evidence and impact at McMaster. The N-of-1 trial tested the patient’s response to two of his four asthma medications. For each drug, the patient alternated the medication and a placebo—neither he nor Guyatt knew which was which—while the patient kept a careful log of his symptoms and ability to breathe.

This N-of-1 trial involved multiple rounds of treatment—a typical strategy today, in which a patient may cycle between treatment and placebo three or four times—and the random, blinded order of the intervention improved the odds that the patient’s response wouldn’t be influenced by a placebo or nocebo effect. Before the trial, Guyatt and the patient both suspected that one of the drugs was the source of the disabling side effects. Yet it turned out that the other—theophylline, which causes extreme reactions in some people and is no longer as widely used—was the culprit. “Once we stopped theophylline, the patient was 100 times better,” says Guyatt.
Guyatt conducted 57 N-of-1 trials during the next few years for McMaster physicians and their patients. The trials produced definitive answers to a clinical or statistical question in 50 cases, and 26 doctors changed their treatment recommendations based on the results. The process was time-consuming and cumbersome, however, and referrals eventually dried up. But word spread, and Eric Larson, now senior investigator at Kaiser Permanente Washington Health Research Institute, created his own N-of-1 service at the University of Washington in 1993, inspired by one of Guyatt’s talks. Larson’s group completed 34 trials before his effort also ended, in this case through lack of funding.
Those issues—too little interest among physicians and not enough financial support—led to a long dry spell for this kind of research. “What Guyatt and Larson attempted to do with N-of-1 trials went against an ingrained mindset that large randomized controlled trials were the only way to evaluate a drug or therapy for safety and efficacy,” says Nicholas Schork, deputy director and distinguished professor of quantitative medicine at the Translational Genomics Research Institute in Phoenix. “There wasn’t much desire to detect individual variability in the response to a drug.”
Those problems were exacerbated by a lack of sophistication in data collection and analysis. That’s different today, says Schork. “In an era where there is now tremendous interest in individual variation as well as better biomarkers and wireless devices for continuous monitoring, N-of-1 trials just make a lot of sense,” he says.
For the latest generation of N-of-1 champions, one of the model’s most compelling uses is to sort out therapy for medical disorders that are highly variable from one patient to another. Obesity, pain, asthma and other conditions can be difficult to treat because patients tend to have idiosyncratic responses to therapies.
Taking on the problem of lower back pain, a recent series of 60 N-of-1 trials compared Swedish massage to yoga and found that the subjects, indeed, differed widely in their responses. “For some, massage dramatically reduced pain and the number of medications they required,” says Karina Davidson, senior vice president of research and director of the Center for Personalized Health at Northwell Health in New York, who conducted the study. “Other patients responded only to yoga, others felt better on both interventions and some responded to neither.” Because the N-of-1 trials tested every patient on each therapy, the patients and their doctors were able to use the resulting data to see whether, and to what degree, these treatments could reduce the need for pain medication.
One compelling use is for medical disorders that are highly variable.
Medically complex patients—often excluded from conventional trials, which try to minimize variables in test subjects—are another example of the variability that makes a good candidate for an N-of-1 study. Alzheimer’s disease, for instance, afflicts older people who are more likely to have multiple additional conditions, one reason that parallel-group RCTs for the disease are hard to implement. “Alzheimer’s is very complex, with symptoms and progression of the disease varying considerably depending on how much amyloid and tau is in the brain, whether vascular or inflammatory factors are driving the disease and so on,” says Arnold. To control for all of that, a conventional RCT would need 2,000 people per arm, he adds.
But N-of-1 trials embrace such variability. Arnold is conducting a pilot study on patients with mild cognitive impairment to determine who might benefit from Ritalin to improve memory and decision-making. The trial is divided into four-week treatment blocks during which each patient takes a placebo or Ritalin for two weeks at a time. Then the blocks are repeated two additional times while patients play daily computer brain games, and periodically take memory and thinking tests. At the end, Arnold will analyze each person’s performance to see who might benefit from the drug.
Such N-of-1 trials might move the needle in finding good, useful treatments for neurodegenerative conditions. With mild cognitive impairment and Alzheimer’s, for instance, behaviors affected by the disease can be hard to standardize across hundreds of patients. But one patient might be measured on her bridge playing ability, while another could be tested on his reaction times in a driving and navigation game. Similarly, neuropsychiatric dimensions of advanced disease, such as agitation, depression or anxiety, can manifest in very personal ways that thwart larger treatment studies. But personalizing the measure—putting a sensor on a suitcase that a patient pulls out of the closet when she feels stressed—can generate relevant data about whether a certain treatment is working.
Such trials might move the needle on treating neurodegenerative diseases.
In all of these cases, the N-of-1 approach can lead to better, individualized treatment recommendations, in part because the trials involve the patient in the process. As with the statin study at Imperial College London, looking at the data can sometimes provide powerful feedback to the patient that leads, in turn, to more satisfaction and better adherence.
The University of Queensland in Australia has embraced N-of-1 trials for a number of conditions, including insomnia, menopausal symptoms, traumatic brain injury, Parkinson’s disease and palliative care. In a series of N-of-1 trials involving 71 patients with chronic pain or osteoarthritis pain, 65% adjusted their pain medications after participating in the trials. One year after enrolling in other personalized trials, seven of 10 participants with attention deficit hyperactivity disorder and 45% of patients with chronic neuropathic pain stayed on the therapies that proved to work best for them during their trials.
One of the most ambitious N-of-1 studies in the United States was designed to help patients with chronic musculoskeletal pain reduce their use of opioids and nonsteroidal anti-inflammatory drugs (NSAIDS), both of which have adverse effects and limited long-term effectiveness. The study randomly assigned 215 people to usual care (continuing pain treatments recommended by their physicians) or to an N-of-1 approach. For N of 1, each person chose two pain treatment regimens from among eight categories that included both drugs and alternative medicine therapies such as massage and exercise. Once those were locked in, a phone app randomized the treatment sequences, notified patients of the treatment they were scheduled to have and reminded them to fill out daily questionnaires about pain levels and side effects.
The patients in the N-of-1 study arm had similar pain scores and patterns of opioid use as patients in the control group, but N-of-1 participants reduced their use of NSAIDS and were more likely to experience a clinically meaningful improvement in pain-related functioning six months out and reported better shared decision-making with their doctors about pain medication. Of the N-of-1 participants who filled out questionnaires after the trial, four in 10 said that data from the trial had given them insight into managing their pain and that they would consider changing their pain medications as a result.
The failure to cut opioid use shouldn’t be laid at the feet of the N-of-1 trial, says Richard Kravitz, the trial’s principal investigator and distinguished professor of internal medicine at the University of California, Davis. Patients saw the evidence that other, less dangerous treatments were just as effective as opioids. But the pull of habit may have been more powerful than convincing data. On the other measures, however, “I think we had clinically important results,” he says.
The N-of-1 model unquestionably requires more effort and more resources than other ways to determine the best treatment for a particular patient, and if the responsibility falls to overstretched primary care physicians, the approach is unlikely to take off. Moreover, the N-of-1 model has its detractors, including pioneer Gordon Guyatt. “Intuitively, N-of-1 trials should be great,” he says. “But if you randomize 50 people to N of 1 and 50 to usual care, there isn’t much of a difference in outcomes.”
For now, Kravitz sees a limited scope for N-of-1 trials. “I think they’ll have niche applications—for statin withdrawal, for example, and perhaps when a patient and doctors are trying to decide between a cheap drug that’s pretty good and an expensive one that looks marginally better in large randomized studies. If an N-of-1 trial finds that the two drugs are comparable for that person, the patient could opt for the cheap drug and save money.”
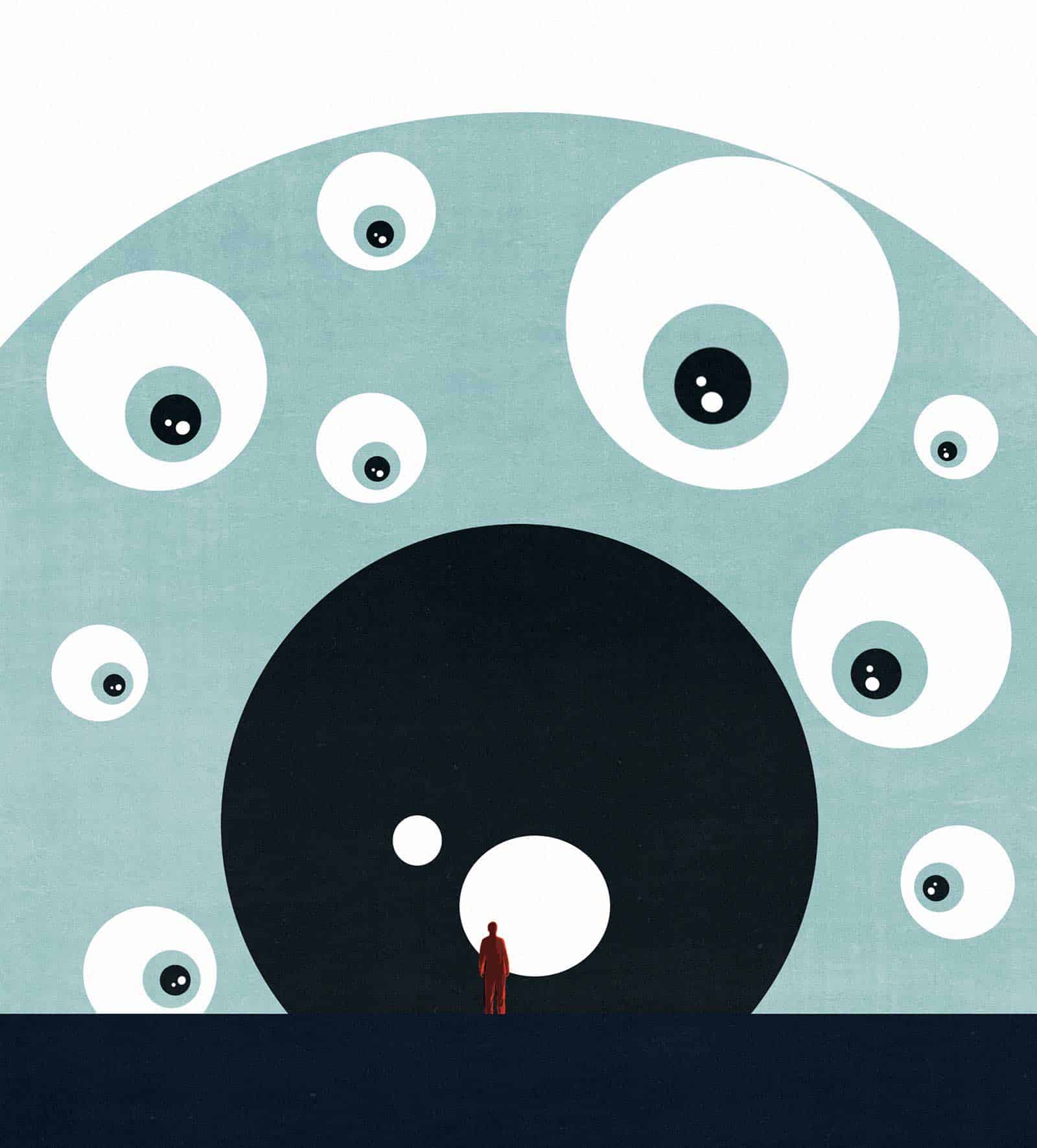
But other N-of-1 research now being done by MGH’s Steven Arnold, Columbia’s Ian Kronish and many others suggests that the impact of individualized trials is only beginning to be explored. For conditions that are notoriously difficult to treat effectively, such as irritable bowel syndrome and dementia, there are broad possibilities for using N of 1 to sort through patients’ individual responses to therapies. “The beauty of an N-of-1 trial is that I can confidently tell a patient whether or not a drug is good for them,” says Arnold. “This approach also eliminates a lot of bias, not only the placebo effect that a patient may experience, but also wishful thinking by a doctor who just wants a patient to get better.”
Karina Davidson at Northwell Health, meanwhile, is creating N-of-1 “kits” that give Northwell physicians and their patients everything they need to systematically test patients’ responses to a series of antihypertensive medications. A second kit, for stress reduction, will be marketed directly to consumers.
And physician Alexander K. Smith, writing in JAMA Internal Medicine, described his experience with an informal N-of-1 trial he designed for himself. After Smith was diagnosed with eosinophilic esophagitis, a chronic immune disease that damages the esophagus and can cause food to get stuck, his gastroenterologist prescribed a “cruel” elimination diet to find the foods that made his condition worse. Conducting his own N-of-1 study, Smith quickly discovered that dairy products were the offending foods. That spared him having to avoid wheat, soy, eggs, seafood and nuts for months, as his doctor had suggested. Rather than abandon N-of-1 trials, Smith urges researchers and clinicians to find their best applications. “Think creatively [to find ways that] N-of-1 trials might simplify treatment regimens, improve patient compliance and reduce health care costs,” he says.
Dossier
“N-of-1 Trials in Healthcare,” Healthcare, March 2021. This special issue includes 13 articles on N-of-1 trials, highlighting pilot studies that focus on a range
of diseases and exploring the barriers and opportunities. The editors emphasize the importance of such trials in a time of movement toward personalized medicine and patient-centered health care.
“Experimental Designs to Optimize Treatments for Individuals: Personalized N-of-1 Trials,” by Karina Davidson et al., JAMA Pediatrics, February 2021.
The article explores the advantages
of personalized trials for children and discusses methodologies through which N-of-1 trials could determine optimal treatment of attention
deficit hyperactivity disorder.
Stay on the frontiers of medicine