Published On July 23, 2007
THE TWO INFECTIOUS DISEASES ARE AMONG THE WORLD’S DEADLIEST, together killing as many as 5 million people a year. Both are caused by viruses identified during the 1980s, and both can be spread by blood transfusions, shared needles and, to varying degrees, sexual contact. Yet in terms of public profiles, they couldn’t differ more. The fight against AIDS long ago became a cause célèbre, the research dollars flow freely, and although there’s still no effective vaccine or cure, advances in treatment have transformed AIDS into a manageable chronic disease. The other killer, hepatitis C, remains relatively obscure. Breakthroughs in understanding the virus, when they come, don’t make the nightly news. But it would be wrong to assume that hepatitis C is a lesser threat.
The World Health Organization estimates that 170 million people, about 2.5% of the world population, are infected with hepatitis C. That is three to four times as many as have the human immunodeficiency virus (HIV) that causes AIDS. And while in the United States sophisticated blood-screening methods and less frequent needle-sharing among intravenous drug users have forced the rate of new infections sharply downward in recent years, an estimated 4 million already harbor the virus, which may lie dormant for decades before erupting into life-threatening symptoms. In the developing world, the disease continues to spread, and the ultimate toll could be devastating. Some who have the hepatitis C virus (HCV) will never know they’re infected. A fortunate few, perhaps 20%, are able to clear it from their systems within the first six months, during the disease’s acute phase, which is usually mild or asymptomatic. But the rest go on to chronic infection. One in five will develop cirrhosis of the liver, a condition in which normal liver tissue is replaced by nonfunctioning scar tissue. And a significant number of those with cirrhosis will develop liver cancer.
Some five in 10 U.S. cases can actually be cured, with the virus eliminated from the patient’s body. That’s true of no other chronic viral condition—not hepatitis B, and not AIDS. But where the need for treatment is greatest—for example, in Africa, where more than 5% of the population is infected and the infection rate continues to rise—the cost of the best therapies puts them out of reach for most of the infected population.
Against this backdrop, remarkable work on the disease is being done. The discovery of the virus, which took more than five years, using untried techniques and requiring frequent leaps of faith, is one of the triumphs of molecular biology. Now, finally, a vaccine may be in sight. Yet despite great progress, hepatitis C remains a real and present danger, particularly in the developing world. It may not be AIDS, but it continues to pose major challenges for medical researchers, and defeating the disease will require time, funding and still more scientific brilliance.

AS EARLY AS THE 1960S, SCIENTISTS KNEW that the liver disease called hepatitis came in two types: infectious, now known as hepatitis A, which is transmitted though food, water and direct contact; and serum, a blood-borne pathogen passed on mostly by needles and sometimes by sexual contact and childbirth. Food-borne hepatitis produced an acute and usually transient infection. The blood-borne version, in contrast, could make people severely ill and often killed them. By 1970, researchers had found an antigen, a kind of protein in infected blood, that indicated the agent was a virus. They named it hepatitis B, and before long, new screening techniques enabled blood banks to eliminate hepatitis B–infected blood.
Other hepatitis viruses were discovered soon afterward. One, now called hepatitis D, works with hepatitis B to produce severe liver disease in patients infected with both. Hepatitis E, like A, is a food- and water-borne virus. Yet it dawned on doctors that these diseases still did not account for all cases of liver disease in patients who had received blood transfusions. After screening eliminated hepatitis B from blood banks, it became ominously clear that another, undetectable agent remained. Not knowing what it was, researchers referred to it in terms of what it wasn’t: “non-A, non-B” hepatitis.
In trying to track down this hidden pathogen, traditional techniques didn’t work. No one could culture it, and while virologist Daniel Bradley at the Centers for Disease Control and Prevention in Atlanta was able to show that non-A, non-B hepatitis could be transmitted to chimpanzees, until the late 1980s that was about all anyone could say for sure.
In 1982, a molecular biologist at a California biotech startup called Chiron joined the hunt. Michael Houghton, in collaboration with Bradley, tried every technique of molecular biology and immunology to search for a protein or genetic sequence that would lead them to the virus. The pair used cutting-edge methods to examine infected blood and liver tissue, looking for genetic material with a high molecular weight that would indicate the presence of a virus. After several years, the researchers had screened 200 million to 300 million genetic sequences, but found nothing.
Then, in 1985, Chiron colleague George Kuo persuaded Houghton to reconsider an approach he had thought too risky. With colleague Qui-Lim Choo, they cloned all the nucleic acids (the building blocks of DNA and RNA) they could find in samples of infected human and chimp blood, the latter provided by Bradley. Then they introduced these genetic sequences into bacterial genomes, so that the bacteria were “persuaded” to manufacture the proteins determined by those sequences. To find the sequences that would yield rare viral proteins, Houghton explains, “we just used infected serum samples to screen lawns of bacteria on dinner plates of culture medium.” This produced extremely smelly dinner plates, because the bacteria was the infamous intestinal E. coli.
Two years and millions of proteins later, the team had found several candidates; it took another year to identify a single clone from infected blood that caused antibodies to bind to it and was not present in normal blood. That clone provided a “handle” to identify the virus and pull it out of infected blood.
Houghton, Choo and Kuo were certain they had found the virus, but they still had to convince the rest of the world. Hepatitis expert Harvey Alter at the National Institutes of Health had developed a famous library of infected blood samples, some containing non-A, non-B contaminated blood. Alter had sent his samples to 40 other research groups, but none had been able to identify the samples with non-A, non-B. “We were the 41st,” says Houghton. “We cracked the code straight away.”
Next, the Chiron group developed a blood test using the clone, which made it possible to screen all donated blood for the virus now known as hepatitis C. By the early 1990s, the U.S. blood supply was clear of the virus, and with an important source of new infections eliminated, the yearly rate of infection has dropped from almost 250,000 to about 25,000. Now the major risk factors for hepatitis C infection in the West are the use of shared needles and other shared drug paraphernalia. Sexual transmission is another source of infection, though a number of studies suggest that in a long-term monogamous union, the risk of passing the infection is remote. The rate of transmission is higher for those who have sex with many different partners.
THE CHIRON DISCOVERY, WHICH EARNED HOUGHTON (on behalf of the team) and Alter the Lasker Prize for medical research (on Alter’s part, not only for providing the crucial blood samples but also for having co-discovered non-A, non-B ), launched wide-ranging efforts to control the hepatitis C virus. Two decades later, advanced therapies can cure the disease in some people. The most effective treatments combine interferon, a naturally produced human immune chemical that fights viral infections, and an antiviral drug called ribavirin, developed years earlier to combat other viruses. Deborah Taylor, a senior investigator at the U.S. Food and Drug Administration, has shown that interferon, on its own, is blocked by the protein envelope that encapsulates the hepatitis C virus; although it is not yet known how ribavirin works or how the two chemicals cooperate, neither can work alone.
Because the body swiftly eliminates injected interferon, the chemical is now typically delivered in “pegylated” form, with the interferon peptide, a short protein chain, attached to a larger molecule that takes much longer for the body to eliminate. Combined with ribavirin, the therapy now cures about 50% of chronically infected hepatitis C patients. It’s still unclear why only some patients respond, though some genotypes, or variants, of the virus respond better than others. But that the treatment prevails at all is remarkable, according to Jules Dienstag of the Massachusetts General Hospital, who notes that this is the first therapy that has managed to cure a chronic viral infection. In many hepatitis C cases, after a year’s therapy, the virus disappears forever.
But this remarkably successful approach has several drawbacks. Of the six distinct genotypes of the hepatitis C virus, genotypes 2 and 3 are the most responsive, with a cure rate of about 80%. But genotype 1, which accounts for 70% of cases in the United States and northern Europe, is more resistant. Moreover, many people don’t tolerate the treatment well. Interferon is usually described as causing “flulike” symptoms, and they can persist for the year it takes to achieve a cure. “Imagine having flu for a year,” says virologist Earl Brown of the University of Ottawa.
Another daunting obstacle is the expense of the therapy, which costs between $15,000 and $20,000 a year. While that may not be prohibitive for some patients in the West, it sharply limits access in the developing world, where the virus continues to spread through a contaminated blood supply and infected needles. In one tragic instance in Libya, hundreds of children in the same hospital were infected with both HIV and HCV through the re-use of improperly sterilized needles. Even more disturbing, some 15% of the Egyptian population, and half of those older than age 50—more than 5 million people—are thought to be chronically infected with type 4 hepatitis C, as the result of contaminated needles used during a massive antischistosomiasis campaign in the mid-1960s.
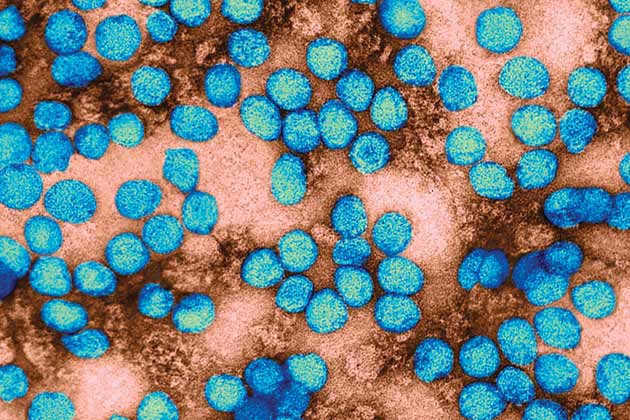
THOUGH IT WOULDN’T HELP THOSE ALREADY INFECTED, a vaccine could slow the spread of hepatitis C and perhaps eventually eliminate HCV as a threat to public health. The vaccine for hepatitis B, introduced in 1982, has greatly reduced the prevalence of that disease. But the protean hepatitis C virus presents special challenges. Once one of the six genotypes establishes a chronic infection in a human host, it keeps mutating, producing what scientists call quasi-species, a swarm of strains that try to outwit the immune system.
Not all portions of the viral genome are equally variable, however. Natural selection has kept some parts quite stable, but others mutate wildly. One such hypervariable region is found in protein E2, part of the envelope around the virus. To study that region and to track the evolution of hepatitis C in a human host, Earl Brown and Yu-Wen Hu of the University of Ottawa have repeatedly tested a patient who, in the beginning, had the virus in his blood but had not yet developed antibodies, which typically show up only after about seven weeks of infection.
Brown and Hu discovered that after the acute phase of the infection, the patient’s immune system had cleared about 95% of the virus. But the remaining 5%, a swarm of viral strains with similar surface proteins, produced a chronic infection. Over time, the surface proteins diverged more and more from those of the original strains, particularly in the hypervariable region of the E2 protein.
Normally, immune cells track down and destroy invading bacteria and virus-infected cells by recognizing them as alien and therefore dangerous. The immune cells “remember” what a particular infection looks like so they can attack if it enters the host again. But with hepatitis C, that doesn’t always happen. Brown and Hu found that in this patient, as viral strains mutated, they came to resemble the host’s own immune proteins and were able to hide from the patient’s immune system. So the body left them alone, and the chronic infection took hold. A Novartis (formerly Chiron) vaccine has been effective in protecting chimpanzees from the disease and was recently studied in a Phase 1 clinical trial at St. Louis University. If such a vaccine shows promise, scientists will need to vaccinate people in high-risk populations—for example, large numbers of intravenous drug users—to see whether they develop hepatitis C less often than do those in a control group.
If this or another vaccine proves safe and effective, it could have its greatest impact in countries of the developing world, particularly in Africa and Asia. But even in the West, and regardless of how soon a vaccine arrives, the impact of the disease will be felt for years to come. People who may have received a blood transfusion before 1992 or injected drugs once at a party 30 years ago could find themselves facing a sometimes untreatable and possibly fatal condition they never knew they had. How much more suffering this rising wave of disease will inflict is still unknown. Two decades of scientific progress has put hepatitis C on the ropes, but the fight continues.
Dossier
“Epidemiology of Hepatitis C Virus (HCV) Infection,” by Theodore Sy and M. Mazen Jamal, International Journal of Medical Sciences, April 2006. An overview of the virus’s worldwide distribution and its various subtypes, as well as a cogent discussion of the risk factors associated with spread of the disease.
“Immunoglobulin mimicry by hepatitis C virus envelope protein E2,” by Yu-Wen Hu et al., Virology, Jan. 12, 2005. This article presents a novel way of understanding how hepatitis C infects: Through a process called molecular mimicry, the virus tricks the immune system by producing proteins that resemble human immune chemicals.
Stay on the frontiers of medicine