Published On January 15, 2009
THE DISCOVERIES OF MANY TREATMENTS for disorders of the brain resulted from happenstance. Iproniazid, the first modern antidepressant, was originally designed as a tuberculosis drug, while a second-generation antidepressant, imipramine, represented a failed attempt to treat schizophrenia. But levodopa, or L-dopa, was meant for exactly the purpose it serves: helping people with Parkinson’s disease overcome the tremors, rigidity and problems with balance that stem from the loss of specialized neurons that produce dopamine. Levodopa replenishes depleted dopamine, a brain chemical crucial for motor control, to dramatic effect.
During his residency in the 1970s, Warren Olanow, now a neuroscientist at the Mount Sinai School of Medicine in New York City, was amazed to see patients, nearly paralyzed by Parkinson’s, stand up and walk after taking the drug. But miraculous as it may be, L-dopa has a serious side effect: dyskinesia, jerky movements that can be as disturbing as the original problems of Parkinson‘s. What’s more, the longer a patient has lived with this progressively degenerative disease, the shorter the drug’s good effect lasts. Still, the temporary balm of L-dopa raises an intriguing possibility that has preoccupied Olanow and others. Could the brain itself be restored, not just by adding a missing chemical but by replacing lost cells and rebuilding decaying neural circuits?
For years the less favored alternative to L-dopa was surgery. To alleviate both the rigidity of Parkinson’s and the dyskinesia caused by L-dopa, the overly active globus pallidus, located deep within the brain in the basal ganglia, was lesioned in a procedure called a pallidotomy. To quell tremors, part of the thalamus, at the top of the brain stem, was destroyed in a thalamotomy. Other brain disorders were treated surgically as well: To subdue severe epilepsy, surgeons targeted the tissue in which seizures arise, usually in one of the temporal lobes. For major depression and other severe psychiatric diseases, the approach was to cut out tissue with a cingulotomy, usually in the anterior cingulate cortex, which was thought to be the emotional center of the brain. Some of these procedures are still used, though recently a few have been supplanted by deep brain stimulation, in which implanted electrodes inactivate specific brain regions.
Cutting away parts of the brain—or turning them off—carries the risks of major surgery and may come with such side effects as memory loss and depression. But until recently, there seemed little point in trying to save aberrant tissue, because scientists thought it was irreparable. As Santiago Ramón y Cajal, who won the Nobel Prize in medicine in 1906, said of neurons, “Everything may die; nothing may be regenerated.” The dogma held that people are born with a given number of neurons that, unlike most cells in the body, cannot divide or be replenished.
That outlook changed when Fred H. Gage of the Salk Institute for Biological Studies in La Jolla, Calif., demonstrated that neurons in certain brain regions can sometimes reproduce themselves, in a process called neurogenesis, raising the possibility that aberrant brain tissue isn’t beyond help after all. “Now, instead of removing or disabling parts of the brain, neuroscientists can think about restoring the malfunctioning organ, either by recruiting the body’s own regenerative capabilities or by adding therapeutic cells and molecules to discrete regions,” says Miles Cunningham, a neuropsychiatrist at McLean Hospital in Belmont, Mass.
The first clinical attempts to restore the brain using transplanted neurons actually started during the late 1980s, even before the revelations about neurogenesis, but the growing understanding of the brain’s innate powers is improving these efforts and expanding the arsenal of restorative neuroscience. So far most studies have focused on such neurodegenerative conditions as Parkinson’s, stroke, spinal cord injuries and epilepsy. But Cunningham is interested in using restorative methods to treat depression and other psychiatric disorders.
PARKINSON’S DISEASE, BECAUSE ITS DESTRUCTIVE effects are quite localized, was a logical first target for testing the possibility of restoring lost brain function. Dopamine-producing neurons in the upper brain stem, in a region called the substantia nigra, progressively die. Normally these neurons extend into structures deep in the midbrain called the striatum (and also the basal ganglia), where they release dopamine. Other neurons in the striatum respond to that dopamine, regulating body movements.
If dopamine-producing neurons could be transplanted into the striatum, scientists speculated, they might accomplish biologically what L-dopa does pharmacologically. Achieving that effect, though, has proved difficult. The most extensive data comes from unblinded trials in which tiny flakes of solid tissue from the fetal brain containing very young dopamine-producing neurons were implanted in the striatum. Researchers were initially encouraged by reports of significant improvement among treated patients. But in 2001 and 2003, two placebo-controlled, double-blind trials (begun in the 1990s) compared the introduction of fetal tissue with sham surgery and failed to show significant differences between the groups. Those studies also revealed an unexpected but familiar side effect: dyskinesia, the same problem encountered by patients on L-dopa. “If results were not any better than with the placebo,“ says Mount Sinai’s Olanow, who led the 2003 trial, “why operate on the brain when there’s a drug that can help just as much?“
Olanow has stopped doing cell transplantation for Parkinson’s, though he might be coaxed into trying again. It appears possible that the early methods used in the trials were partly to blame for the trials’ failure and that newer techniques could prove more successful. For one thing, tissue flakes don’t appear to meld as well in the brain as do fetal neurons that are injected in a suspension. Recent trials have used suspended cells, but definitive results are not yet in. Adult stem cells, which weren’t available when the trials began in the 1990s, as well as other immature, undifferentiated cells (further along in the progression from stem cells to specialized cells), might work best of all, but so far that’s still hypothetical. Olanow also notes that even a successful approach would not alleviate the symptoms that aren’t related to dopamine, such as falling and dementia.
Another reason the early trials failed may be that even though the damage wrought by Parkinson’s happens in only a few brain regions, within those regions the brain degenerates in highly individualized patterns. So it’s possible that therapy needs to be customized, suggests Stephen Dunnett, a cell transplantation researcher in Cardiff, Wales, who thinks that distributing new cells to correspond to each individual’s disease pattern—another untried approach—might improve results.
Refined surgical techniques could also help. Some trials may have plunked too many cells into too concentrated a location using a thick, rigid cannula that traumatized the brain and elicited an inflammatory response that killed many of the new cells. “Cell transplantation requires a different technique from clinical neurosurgery, which aims to get in and out of the brain as quickly as possible,” Dunnett says. “These fragile cells need to be injected very slowly. They get smashed up if you push them into the brain too fast.” Those realities might favor newer techniques and devices such as an ultrathin, flexible microinjection tool that Miles Cunningham has developed.
BUT IT’S NOT ENOUGH JUST TO ADD neurons to the brain. The immature cells have to differentiate into cells with the correct characteristics, such as neurons that produce dopamine. Then they need to migrate to where they are needed in complex brain circuitry and form connections with the correct combination of other neurons. Only those that make good connections can survive, and then they have to function, explains Jeffrey Macklis, director of the Massachusetts General Hospital–Harvard Medical School Center for Nervous System Repair.
To help that happen, scientists need to remind the ailing brain how it formed functioning neural circuits in the first place. “We now know that, as an embryo develops, there’s an orchestrated sequence of brief, interacting molecular signals that controls which of many possible developmental paths the newborn neurons take,” Macklis says. “After a while, the developmental score falls silent in most areas, but in a few regions where adult neurogenesis occurs, it is replayed.”
Those areas are normally confined to one small region of the hippocampus (the dentate gyrus) involved in learning and memory, and to the olfactory bulb, which responds to odors. However, “progenitor” cells (often called adult stem cells) capable of differentiating into several types of higher-level neurons also exist in other brain areas, in which they have untapped restorative functions. Macklis is trying to exploit those functions by learning the developmental score for specific neuron types and then activating them, along with the signaling molecules and other factors—for growth, protection and gene transcription (turning genes on and off)—that help neurons survive, specialize and migrate.
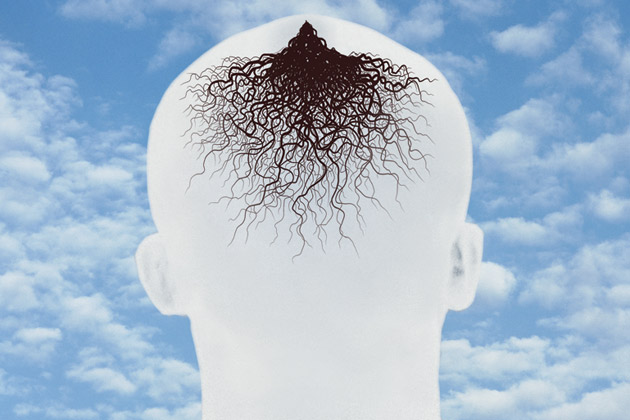
In the hippocampus, neurogenesis is stimulated by exercise, antidepressants and physical and cognitive therapy. Seizures, strokes and Alzheimer’s and other degenerative diseases may also result in the creation of a small number of new nerve cells, though in a disorganized and ineffectual way. It’s as if an injured or diseased brain were calling upon its inner reserves—the progenitors—to heed its distress. “But the complexity of injury or degeneration in such disorders confuses the progenitor response, and it doesn’t lead to the birth or incorporation of functional neurons,” Macklis says.
His group has shown that it’s possible to direct the precise repair of specific brain circuits. In experiments with mice, the team implanted progenitor cells into the cerebral cortex—which doesn’t normally support new neural growth—and provided developmental signals instructing the new neurons to form connections with distant parts of the brain. Macklis spurred the reactivation of those signals by inducing the cell-suicide program called apoptosis in one population of neurons at a time. Healthy neighboring neurons that lost their circuit partners emitted a call to arms that the injected progenitor cells heeded. That caused the new neurons to fill the old ones’ roles and to restore the lost connections in the neural circuitry. This works, Macklis says, because only one neuron type is formed at a time. He found he could also activate those signals to induce existing precursors in the mouse cortex to undergo neurogenesis and extend their own connections.
Macklis is now focused on learning the signals to induce neurogenesis in the types of neurons that degenerate in amyotrophic lateral sclerosis and Huntington’s disease or that are damaged in spinal cord injuries and in some forms of cerebral palsy—work that has progressed to animal studies.
Despite these advances, Macklis thinks that inducing neurogenesis to good clinical effect in people lies further in the future than cell transplantation. Already, though, knowledge gained from studying neurogenesis is improving cell transplantation techniques and could enhance their therapeutic effects. In addition, newer transplantation studies are adding protective agents to try to prevent damage rather than just repairing it once it has occurred.
This accumulating knowledge also means that cell transplantation is no longer simply about replacing lost cells with cells that perform the identical function. It may be possible to add cells that perform new roles. For example, some transplanted cells could produce growth signals to encourage the formation of neural networks, while others could generate protective factors to improve the survival prospects of newborn neurons, and still others might manufacture hormones and other brain chemicals to stabilize moods. Eventually, Dunnett suggests, cell transplantation coupled with gene therapy might be able to keep a neurodegenerative disease from progressing.
The idea that such ongoing therapies are needed was bolstered by Olanow’s May 2008 report of a Parkinson’s patient who had received a transplant of fetal tissue 14 years before her death in 2007. At first doctors found her symptoms had been dramatically reduced, but then her condition worsened, and she continued to deteriorate until her death. A postmortem study revealed that the grafted cells had indeed formed working connections with the brain’s circuitry. But eventually the new cells began to show the same pathology—sticky clumps of protein called Lewy bodies—that characterizes Parkinson’s.
“This tells us a great deal about the disease: that it results from an ongoing process, not a one-time event, and that it can overtake even implanted neurons,” Olanow says. Finding out why that happens is the current focus of his research.
It’s too early to tell whether a similar process overwhelms implanted neurons in Huntington’s disease (trials to treat that condition don’t yet have such long-term follow-up) or will thwart attempts at restorative neuroscience for other conditions. Even so, many people might consider the alleviation of symptoms for several years at least a partial success.
THE PHYSICAL DYSFUNCTIONS OF PARKINSON’S—among them, tremors, rigidity and problems with balance—that have been the subject of human trials of restorative neuroscience are debilitating. Even worse are cognitive deficits and mood disorders. The same holds true for Huntington’s disease and many other neurological and psychological disorders. In cognition, neural circuits and the interplay of brain chemicals are devilishly complex, and those involved with mood and emotion are even more elusive. But new techniques in restorative neuroscience may help researchers learn more about these brain systems and even to intervene therapeutically.
In late 2007, McLean’s Cunningham published a preliminary study applying the transplantation of neural stem cells to a neuropsychiatric disorder. In a rat model of depression and anxiety, Cunningham had used various growth factors to cue the stem cells to differentiate into two types of neurons. One type of cell produced serotonin, the “feel good” neurotransmitter that Prozac and other antidepressants elevate; the other made dopamine, which also plays a role in mood.
Using his intracerebral microinjection instrument, Cunningham infused these neurons into an area of the brain related to emotions—the rat version of the human anterior cingulate cortex, which has shown irregular activity in imaging studies of depressed patients. Deep brain stimulation usually targets the anterior cingulate cortex, which in past years has been surgically altered in cingulotomies to treat major depression.
Six weeks after infusing the new neurons, Cunningham ran his rats through a forced swim test, a standard procedure for inducing “learned helplessness,” a well-studied surrogate for depression in humans. He compared the performance of rats that had received transplanted cells with that of other groups that had gotten sham surgery, antidepressants or no treatment. Only the rats on antidepressants and those with the transplanted serotonin and dopamine neurons rebounded from their depression, in equal measure. Postmortems showed that a greater proportion of the implanted cells survived than has been typical of cells sent into the brain, and Cunningham thinks that might be because his device, with a needle the diameter of a horsehair, caused less damage to brain tissue than the traditional coffee-straw-size wand. Molecular and genetic analyses also indicated that the cells had indeed produced the desired neurotransmitters, calming the activity of fear circuitry (in the amygdala) that increases during anxiety and depression.
“So we think it’s the activity of the transplanted cells that resulted in the rats’ behavioral improvements,” Cunningham says. “We’re very excited because this is the first time that embryonic stem cells have been used to achieve a therapeutic effect in a psychiatric disease.” Now Cunningham’s team is expanding its studies to investigate links among stress, fear and depression. Eventually this work could open the door to entirely new methods for treating mental illness, he says. These approaches to restorative neuroscience still require surgery to get therapeutic agents into the brain. But today’s surgery is intended to rebuild neural circuits, not dismantle them, and the possible uses for these therapies are expanding as scientists learn more about how the normal brain functions and how diseases and disorders affect specific brain regions and their connections to other regions.
In the passing era of neuroscience, lesion studies in animals—in which discrete brain sections were disabled to help researchers understand their functions—and studies of people with localized brain damage contributed great swaths of understanding about the brain. As a result, physicians were able to treat severe disorders surgically or with deep brain stimulation. Now that process could be reversed. Investigations that consider the ways that manipulating brain circuitry affects behavior, cognition and mood may ultimately lead to ways to repair actual lesions and restore normal activity to the misbehaving brain.
Dossier
“Adult Neurogenesis and Cellular Brain Repair With Neural Progenitors, Precursors and Stem Cells,” by U. Shivraj Sohur, Jason G. Emsley, Bartley D. Mitchell and Jeffrey D. Macklis, Philosophical Transactions of the Royal Society: Biological Sciences, September 2006. A discussion of how disturbances of the brain’s natural ability to repair itself contribute to neural disorders.
“Stem Cell Transplantation for Neurodegenerative Diseases,” by Anne E. Rosser, Rike Zietlow and Stephen B. Dunnett, Current Opinion Neurology, December 2007. The authors present early evidence that adult neural stem cells and other immature neurons can be transplanted into selected brain regions to restore functions lost as a result of neurodegenerative diseases.
“Antidepressant Effect of Stem Cell-Derived Monoaminergic Grafts,” by Miles G. Cunningham et al.,NeuroReport, October 2007. This study of rats extends the hopes for cell transplantation in restorative neuroscience to a neuropsychiatric condition: depression.
Stay on the frontiers of medicine