Published On February 12, 2016
TWICE A WEEK John Farris pulls up to a two-story home in Fort Worth, Texas. Farris is a paramedic but he drives a Ford Fusion, not an ambulance, and instead of coming to take 42-year-old Christopher Collins to the emergency room, he’s there to make sure Collins stays out of it. During today’s visit, Farris checks his patient’s vital signs, but on other visits he might draw blood and take an electrocardiogram. He records the data on his tablet computer, which gives him access to Collins’s medical records, and he sends information to Collins’s doctors. Farris reviews the list of medications Collins is taking, checks his home for hazards that could lead to falls or other problems, and works with him on meal plans to reduce the amount of salt and sugar he consumes.
The house calls have helped Collins, who is a Protestant minister and foster parent to six children, manage a complicated set of medical problems that includes congestive heart failure and kidney disease. Since open heart surgery in 2015 he has been to the emergency room six times, but now, a month after his latest hospital stay, Collins says he’s feeling “100% better.” One time he was on the verge of going to the ER because he was short of breath and retaining fluids—possible signs of congestive heart failure. But Farris came to see him and correctly identified an upper respiratory infection, for which Collins was able to get treatment at a local urgent care center. “A lot of times I haven’t been able to reach my primary care physician, but when I called John, he came immediately, and I ended up not going to the hospital,” Collins says.
Scheduled house calls may seem like a throwback to an earlier era, but they’re an essential part of an innovation known as mobile integrated health care and community paramedicine (MIH-CP), or simply community paramedicine. Farris works in a program launched by MedStar Mobile Healthcare, an emergency services agency that works with several local health care groups. As a paramedic, Farris had been trained to aid accident victims and perform emergency care, but MedStar gave him the training to deliver primary care as well. And while MedStar continues to provide traditional ambulance services in 15 Texas townships, it has also partnered with hospital chain JPS Health Network and two other local hospitals, an independent physicians group, two hospice providers and a home health care agency. Those providers pay MedStar and its specially trained paramedics to coordinate care for patients and to help keep them out of the hospital.
Paramedics and emergency services are speedy, mobile and around the clock—which is why medical systems, facing gaps in care, especially in patients’ homes, have started turning to them for answers. “Community paramedicine programs have grown exponentially in recent years, with pilot programs focusing on a wide variety of issues,” says Karen Pearson, a policy analyst at the Maine Rural Health Research Center at the University of Southern Maine in Portland. She’s studying a dozen three-year pilots in Maine, most of which are rural. But there are also trial programs in New York City, Chicago, Boston and the San Francisco Bay Area, which all grapple with overcrowded emergency rooms and lots of unnecessary ambulance trips.
According to a 2015 survey by the National Association of Emergency Medical Technicians (NAEMT), more than 100 emergency medical services agencies in 33 states and the District of Columbia have launched MIH-CP programs, and another study found that virtually every state is at least looking into this approach. During home visits, EMS providers deliver health education and help patients navigate the health system and manage chronic diseases. A primary goal has been to follow up after patients have been discharged from the hospital and help avoid readmission. They also transport patients to doctors’ offices, urgent care facilities, and mental health or substance abuse treatment centers—and while using trained paramedics to act as taxi drivers may seem lavish, it’s still much less costly than an ER visit.
The Affordable Care Act and its mandate to boost access to care, improve quality and control costs is a big impetus for this approach. “Community paramedicine could result in a huge shift in the way we provide care,” says Alasdair Conn, a physician and chief emeritus of emergency services at Massachusetts General Hospital. But like many other hospitals, MGH is taking a wait-and-see approach, given the scarcity of published data confirming the safety, cost-effectiveness and feasibility of MIH-CP programs. The new models also face regulatory and reimbursement hurdles. The Centers for Medicare and Medicaid Services and private health insurers pay for emergency medical services only if patients are transported to the hospital. Pilot programs, meanwhile, are funded by foundations, federal agencies and other groups that have a stake in seeing whether MIH-CP can work as well as its proponents believe it can. But at some point insurers will have to change their policies if this model is to have a major impact.







8:30am
Medstar community paramedic John Farris begins his 12-hour shift. He speaks with a dispatcher to discuss the day’s schedule, which includes in-home visits to five patients, one every two hours.
9:20am
Farris tests blood samples for his first patient, Christopher Collins. Within minutes, a digital readout from a portable analyzer provides data on blood values, which can indicate heart or kidney problems.
9:35am
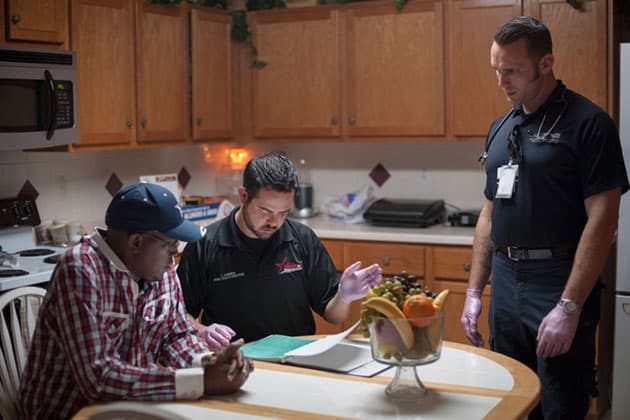
During Each visit, Farris reviews the daily log Collins keeps to track his meals and weight. These “tabletop” encounters often lead to longer conversations about ways to better manage a condition through diet, nutrition or exercise.
11:15am
Joseph Godwin (far right), a medical student at Texas College of Osteopathic Medicine in Fort Worth, helps Farris conduct a physical assessment on Pamela Ferguson, the second patient of the day, as part of the school’s new rotation in mobile integrated health care.
11:45am
Farris monitors the progress that Ferguson, who suffers from heart failure and diabetes, has made in her ability to walk and engage in other activities of daily living. Through Farris’s guidance and working with a physical therapist, she no longer needs a wheelchair and has lost 60 pounds.
1:45pm
Farris consoles Lupe Rascon, whose 85-year-old mother, Lily, suffers from cancer and is being transferred to home hospice care after a month with MedStar. “Compassion is often the forgotten protocol,” says Farris, “and you do get close to patients and their families.”
3:30pm
Farris records an ekg for his next patient, who suffers from heart failure. He will e-fax it to the patient’s physician and cardiologist for a consultation. Most community paramedics rely on comprehensive care plans developed with the patient and family in conjunction with the primary care physician or other specialists.
6:00pm
Farris records an ekg for his next patient, who suffers from heart failure. He will e-fax it to the patient’s physician and cardiologist for a consultation. Most community paramedics rely on comprehensive care plans developed with the patient and family in conjunction with the primary care physician or other specialists.
MODERN PARAMEDICINE began in the 1960s, largely as a response to carnage on the nation’s highways. Rescue squad personnel, police, firefighters and ambulance attendants began to get standardized emergency training, and most of the nation’s 20,000 EMS agencies still focus on their original mandate, responding quickly to accidents and emergencies, stabilizing patients and rushing them to emergency rooms. “You call, we haul—that’s the traditional role of the paramedic,” says Matt Zavadsky, public affairs director for MedStar. And although a report from the U.S. Department of Transportation in the mid-1990s called for integrating EMS into the community and providing preventive care, community health interventions and management of chronic illnesses, that didn’t happen.
Now, however, demographic factors and other forces may converge to expand the role of EMS. Studies suggest that at least one-fifth of the estimated 240 million annual calls to 911 don’t qualify as medical emergencies but instead involve patients with chronic diseases or with mental health or social issues who need help managing their condition rather than a trip to the emergency room. A 2006 Institute of Medicine report, “Emergency Medical Services at the Crossroads,” notes that local EMS systems often “are not well integrated” with other groups providing health care.
Community paramedicine was pioneered in rural areas lacking adequate numbers of primary care doctors. A pilot program in New Mexico, launched in the mid-1990s, failed within five years, but many others showed considerable promise and served as models. Eagle County Paramedic Services—which serves patients across 1,600 square miles of Colorado, an area with a full-time population of 55,000 that triples in winter months when skiers arrive—studied a Nova Scotia program that had been operating since 2000. Using $500,000 in grant money, they began their own five-year community paramedicine program in 2010. Today the Eagle County paramedics visit patients to draw blood, provide wound care, follow up on hospital discharges and look for possible overlaps in the medications patients have been prescribed—a robust combination of services that has led to Eagle County’s program being dubbed “community paramedicine on steroids,” says Christopher Montera, the group’s chief of clinical services and assistant CEO.
Meanwhile, urban and suburban communities have also begun to experiment with MIH-CP programs. In Fort Worth in July 2009, MedStar paramedics began to make house calls to regular emergency room visitors after an internal audit revealed that 21 patients had been transported to local ERs 800 times during a 12-month period at a cost of nearly $1 million—largely unreimbursed because most of the patients had no health insurance. MedStar has since launched six ongoing programs, including one that enrolls into their EMS loyalty program those it calls “frequent fliers,” patients who have called 911 at least 15 times in a three-month period. Specially trained paramedics educate these patients and connect them to available resources in the community. MedStar also has a program that diverts 911 callers with less severe issues to a nurse who helps the patients find alternatives to the ER. These services have become the fastest-growing part of their business, and in 2013, after 27 years as MedStar Emergency Medical Services, the company renamed itself MedStar Mobile Healthcare.
MEDSTAR’S PARTNERSHIP WITH a local home health agency, Klarus Home Care, marks one of the first alliances between such groups. Klarus pays MedStar to provide care coordination services for Klarus patients who call 911 in MedStar’s service area. On the scene, MedStar paramedics work with clinicians by phone to administer home care to patients and determine whether they need to go to the ER. Home health agencies, whose visiting nurses provide medical care in patients’ homes, have good reason to get involved—like hospitals, it is possible that they could begin to be penalized if Medicare patients are readmitted to the hospital.
But some home care providers are worried that an expanded role for paramedics bumps into their own. In Colorado, Eagle County’s community paramedicine pilot had to take a seven-month hiatus after it was seen to be encroaching on home health professionals’ turf by performing scheduled home visits. The state’s department of public health ruled that the EMS group would have to be licensed as a home health provider and its paramedics would need additional education and training. Similarly, the National Association for Home Care & Hospice and the Minnesota Nurses Association tried to block the expansion of community paramedicine programs in that state.
The laws and regulations governing EMS licensing and the scope of practice vary from state to state. Most training for paramedics who take on the expanded duties is provided through specialized online instruction, the pilot programs or courses at local community colleges. “Community paramedicine, which involves chronic disease management, health teaching and counseling, is distinctly different from traditional EMS, and that presents challenges,” says Janet Haebler, senior associate director of state government affairs for the American Nurses Association, which is pushing for standardized training, education and credentialing for those involved in MIH-CP.
Some states, meanwhile, are working to overcome regulatory barriers. In 2012, Maine passed an exception to existing law, authorizing the dozen community pilot projects now under way. And although California law normally requires that paramedics take 911 callers only to emergency rooms, that state, too, found a way to authorize the launch last year of a dozen paramedicine programs. Massachusetts, meanwhile, passed legislation in August that enlarged the scope of practice of community paramedics while also calling for more training and education.
AS PILOT PROGRAMS AROUND the country work out snafus and collect data, those who are launching new efforts turn to existing experiments for help. Last spring, for example, Beth Israel Deaconess Medical Center in Boston began a trial program with Cataldo Ambulance Service, using funding from the Leon Lowenstein Foundation to supplement a federal grant supporting the hospital’s program to reduce readmissions for high-risk Medicare patients. In getting the Beth Israel Deaconess experiment up and running, physician Julius Yang sought out EMS providers in the Maine pilot groups for advice and insights. And MedStar has hosted 160 EMS programs from 42 states with the same purpose.
So far, though, there’s not a lot of hard data to validate the performance of MIH-CP programs. “There are plenty of national reports encouraging the use of community paramedicine, but the peer-reviewed literature is sparse regarding evaluations and outcomes,” says Pearson at the University of Southern Maine, whose 2014 study identified some of the challenges of integrating community paramedics into health care delivery systems. In her ongoing analysis of the Maine programs, she has found that those making the most progress are affiliated with a hospital system that can serve as a source for referrals. Other pilots have struggled with low patient volumes because participating physicians weren’t consistently utilizing their services. “This is a change in the primary care practice model. Physicians aren’t used to being linked to EMS,” she says.
A recent independent account of MedStar by the U.S. Health and Human Services Agency for Healthcare Research and Quality reported that its programs have significantly reduced 911 calls, leading to declines in EMS and hospital emergency room expenditures and reducing ER logjams. Based on two years of data, there was an almost 70% reduction in 911 calls and ER visits for “frequent flier” patients, and admissions to the hospital fell 45%. Overall, at an annual cost of about $560,000, the MedStar programs have saved more than $10.8 million in health care payments and reduced 911 calls by enrolled patients 86%, according to MedStar.
Similarly, during a three-year period, the Eagle County community paramedicine program calculates that it has saved $412,000 by eliminating at least 800 unnecessary visits to physicians’ offices, emergency rooms or nursing facilities, according to the program. An MIH-CP program in Reno, operated by the Regional Emergency Medical Services Authority, has also achieved solid results, with an evaluation by the University of Nevada showing savings of $5.5 million in 2013 and 2014. The program helped avoid 3,483 emergency department visits, 674 ambulance trips and 59 hospital readmissions, according to the preliminary data, says Trudy Larson, director of the university’s School of Community Health Sciences. And North Shore-LIJ Health System on Long Island has spent $400,000 on a community paramedicine pilot that it started in late 2013 for about 1,300 high-utilizer Medicare and Medicaid patients. In its first 19 months, the pilot saved more than $4 million in Medicare payments, based on avoided emergency room transports.
Yet despite promising results, the programs are unlikely to expand broadly without a change in federal reimbursement policies. Medicare, Medicaid and most private insurance plans still will pay EMS providers only to transport patients. Among the states, only Minnesota has passed legislation to reimburse paramedics for nontraditional services through its Medicaid program. And while MedStar and a few other programs have found partners to help them become financially self-supporting, most pilots continue to rely on federal, state and nonprofit funding.
The Centers for Medicare & Medicaid Innovation have delivered $30 million to MIH-CP pilot programs in Connecticut, New York and Arizona. But Bryan Choi, a physician and assistant professor of emergency medicine at Brown University’s Alpert Medical School in Providence, notes that implementing even a small pilot program can be a major effort and a significant risk because of the lack of normal reimbursement. Choi has been working with a dozen groups in Providence, including community officials, EMS providers, home health agencies and social services for more than two years to prepare a MIH-CP trial program to be launched this year.
Providers in Providence need a new response to the rising cost of hospitalizations, new guidelines about readmissions, and the need to manage care in the home. Like administrators of community paramedicine programs around the country, Choi is optimistic about the work but realistic about the hurdles ahead. “Like any new initiative in medicine, you have to go about this very slowly,” he says.
Dossier
“The Evidence for Community Paramedicine in Rural Areas: State and Local Findings and the Role of the State Flex Program,” by Karen Pearson et al., (Flex Monitoring Team, 2014). One of the first in-depth studies that defines and evaluates the role and challenges of community paramedicine. It also describes 12 pilot programs under way in Maine.
“Mobile Integrated Health Care and Community Paramedicine: An Emerging Emergency Medical Services Concept,” by Bryan Y. Choi et al., Annals of Emergency Medicine, July 2015. This critical analysis by physician-scholars looks at existing programs and concludes that more study is needed to support both the clinical and economic benefits of community paramedicine services.
Stay on the frontiers of medicine
Related Stories
- Mobile Aid
In 1792, a clever French army surgeon devised the “the flying ambulance.”
- Defined: Community Paramedicine
A new approach to in-home care turns to EMS providers.
- Sick of Waiting
Emergency room jam-ups threaten patients, inflate costs and disrupt hospital operations. Small fixes might solve this big problem.