Published On September 22, 2013
BLOODLESS SURGERY IS SOMETHING OF A MISNOMER. There’s bound to be bleeding, even when an operation is performed using minimally invasive techniques that require only small incisions. What bloodless surgery strives for, however, is to limit any transfusion of banked or donated blood. When patients, usually for religious reasons, can’t accept someone else’s blood, a series of other measures may be put in place. Well ahead of time, blood tests for anemia can determine whether a patient needs to receive intravenous iron to increase the number of red blood cells. Before surgery, physicians often order a unit of whole blood removed from a patient and replace it with saline intravenously to restore the volume of circulating blood, then the unit is reinfused post-surgery. Clotting medications can be given, and the surgical team may use a cell saver, a machine that suctions, purifies and recycles blood lost during surgery. And post-surgical blood drawing is minimized.
For Mark Sanchez, a 61-year-old Jehovah’s Witness in New York City, the willingness of New Jersey’s Englewood Hospital and Medical Center to take such measures made him choose that hospital over more famous institutions in Manhattan. He signed documents confirming that because of his religious beliefs, he’d rather die than undergo a transfusion. The four-hour operation, for an obstructed bowel, went well, and Sanchez was home five days after surgery. Within a couple of weeks, he was back at work. “Everyone was surprised how quickly I recovered, and I basically haven’t had any problems,” says Sanchez, a clinical social worker.
Most people are willing to accept blood transfusions, which save the lives of as many as 4.5 million Americans each year. They are crucial in some operations or after accidents or other trauma. Yet while the risk of receiving contaminated blood—a real danger during the early days of the AIDS epidemic—is very low today, there are other concerns about the safety, cost and effectiveness of routine transfusions, and some people believe bloodless medicine strategies should become mainstream. Blood “management”—using blood carefully but appropriately, with the goal of minimizing transfusions—is good practice for all patients, says Harvey G. Klein, chief of the National Institutes of Health’s Department of Transfusion Medicine.
Large-scale studies suggest that blood is given too often, and last year, the American Medical Association and the Joint Commission identified transfusion as one of the five most overused medical treatments. A growing body of research links transfusions to serious potential complications, including immune system suppression, inflammation, renal and pulmonary injury, and even death. Studies show that transfused patients also have longer hospital stays and more time in intensive care units. Moreover, with donated blood increasingly expensive and sometimes in short supply, hospitals have economic motivations for restricting transfusions. “Blood management seems to be coming of age,” says Lawrence Goodnough, director of transfusion services at Stanford University Medical Center. “But I think a lot of the momentum may be due to hospitals’ budgetary concerns.”
The Stanford hospitals launched a formal blood management program in July 2010, and there are now an estimated 200 blood management initiatives, with more in development at an estimated 100 hospitals. “Some, like ours, are comprehensive, while others may use just one or two strategies, such as cell salvage techniques or presurgical anemia management,” says Patricia Ford, medical director of the Center for Bloodless Medicine and Surgery at Pennsylvania Hospital in Philadelphia. It’s one of about 100 centers recognized by the community of Jehovah’s Witnesses as specialists in bloodless surgery.
Advocates argue that blood management offers a rare opportunity to improve outcomes, reduce risks and minimize costs all at the same time. Yet while some hospitals have been voluntarily implementing transfusion guidelines based on recommendations from medical societies or other authorities, many more have held back. “Most hospitals don’t have the time, the money, the expertise or the tools to put comprehensive programs in place,” says Tim Hannon, a physician and founder of Strategic Healthcare Group, a blood management consulting firm based in Indianapolis that has worked with more than 100 hospitals.
AFTER WORLD WAR II, the ready availability of a safe blood supply transformed modern medicine, and during recent decades, blood transfusions have skyrocketed, more than doubling between 1997 and 2009 to a high of more than 15 million units of whole blood and red blood cells transfused annually. The United States uses far more blood—49 units per 1,000 patients—than do the United Kingdom and Canada, which average just 32–35 units per 1,000 patients. Aryeh Shander, executive director of Englewood Hospital’s Institute for Patient Blood Management and Bloodless Medicine and Surgery, argues that the U.S. figure is too high, reflecting a gap in medical education and clinical research. Physicians get just a few hours of medical school training in blood transfusion medicine, even though transfusions are hospitals’ most frequently performed invasive procedure.
For decades, most decisions to transfuse blood have been based on the “10/30” rule. The goal has been to maintain the concentration in blood of hemoglobin, a protein that carries oxygen, at 10 grams per deciliter or higher, and to keep the hematocrit—a measure of the proportion of your total blood volume that is composed of red blood cells—at 30% or higher. The average hemoglobin level is 14 grams per deciliter for healthy adult males and 13 for adult women, and the normal hematocrit range for both men and women is well above the 39% level. It has been thought that when surgery or an injury dilutes the blood so that those values drop below the 10/30 threshold, a transfusion is needed to ensure that the blood is able to distribute a healthy amount of oxygen to body tissues.
That recommendation was first established in 1942 by Mayo Clinic physicians John Lundy and R. Charles Adams. But it was based only on their experience with patients, and it would be decades before researchers provided any scientific support of 10 g/dl as the minimum hemoglobin concentration needed for the body’s organ system to function optimally.
But was there really anything magic about 10 g/dl? The discovery in the 1980s that HIV/AIDS could be transmitted through blood was a major catalyst toward blood conservation. Suddenly, many patients who weren’t Jehovah’s Witnesses also were opting against transfusions. Better screening of blood donors and improved lab tests for detecting not only HIV but also other pathogens have alleviated most such fears, and fewer than 1% of patients who receive transfusions suffer severe adverse effects, according to the 2011 National Blood Collection and Utilization Survey.
There are, however, questions about how long blood can be safely stored. For decades, the Food and Drug Administration has required that refrigerated red blood cells be discarded after 42 days, and recent research suggests that stored blood may degrade sooner, and in ways that may be harmful. In a 2008 study published in The New England Journal of Medicine, heart surgery patients who received blood stored more than 14 days fared worse—with more complications and higher death rates in the hospital and long term—than those who received newer blood. In another study this year, published in Anesthesia & Analgesia, researchers at Johns Hopkins found that red blood cells stored for more than three weeks began to lose the normal properties of the cell membrane, changes likely associated with reduced oxygen delivery. Steven Frank, lead author of that study and medical director of the Johns Hopkins Hospital blood management program, contends that it may be suboptimal to transfuse older blood, although blood banks routinely use the oldest blood first. Results of two large randomized trials may soon provide more definitive answers about stored red cells.
BEYOND T whether transfused blood is safe are perhaps even more crucial issues about when and under what circumstances transfusions actually help patients—and when they’re not needed. Jehovah’s Witnesses have served as an important cohort to study, and in 1977, heart surgeon Denton Cooley, founder of the Texas Heart Institute, published seminal research in the Journal of the American Medical Association analyzing more than 500 cardiac operations that were safely performed in that population without transfusions. A 2012 study in JAMA Internal Medicine by researchers at Cleveland Clinic, tracking patient outcomes over almost three decades, concluded that 322 Jehovah’s Witness patients survived cardiac surgery at a similar rate to those in a group that did get transfusions. They also had a better one-year survival rate. Moreover, the Jehovah’s Witness patients had fewer complications, such as risks of additional surgery, heart attacks, kidney failure and infections.
Broader studies have produced similar conclusions. In research involving more than 5,000 heart surgery patients published last June in The Annals of Thoracic Surgery, those who received blood transfusions had a higher risk of infection, and each unit of blood that a patient received was associated with an increased risk by 29%. A 2008 analysis in Critical Care Medicine evaluating the risks of transfusions for nearly 275,000 patients in 45 studies found that transfusions were associated with significantly higher rates of infection and mortality. One potential problem is fluid overload; extra blood can overwhelm the heart’s ability to pump it through the body, and circulatory overload is a leading cause of transfusion-related death. Still, not everyone is convinced that transfusions themselves lead to the medical problems found in these studies. Patients who get transfusions tend to be sicker and more prone to infection than those who don’t need additional blood—factors that may not be captured in recent research.
Guidelines from four medical societies and the AABB (formerly the Association of American Blood Banks) generally agree about when transfusions are called for—when a patient’s hemoglobin level falls below 7 to 8 grams per deciliter—and they recommend against giving blood to patients whose levels are above 10 g/dl. That leaves a significant middle ground about which there’s no consensus, though the Critical Care Medicine study found scant evidence that routine transfusions help stable patients whose hemoglobin readings are greater than 7 g/dl.
Other studies have shown that transfusion practices vary widely among institutions, physicians and procedures. In research published in the July 2012 Anesthesiology, Frank and his colleagues found wide variations within their own institution in an evaluation of the records of more than 48,000 surgical patients hospitalized from February 2010 to August 2011. Just shy of 3,000 patients were given blood transfusions during surgery, with two-thirds of those receiving two or more units of blood. But transfusion rates varied as much as threefold among physicians performing the same procedure, and there was no correlation between the amount of blood transfused and how sick patients were or how much blood was typically lost during particular types of surgery, Frank says. “We were surprised the variation was so large,” he adds. “The problem is that the guidelines for transfusion aren’t well known, and physicians tend to err on the side of giving more blood than necessary.”
Even elderly or other high-risk surgical patients may need fewer transfusions than they normally receive. A 2011 study in The New England Journal of Medicine focused on more than 2,000 patients with an average age of 81 and a history or risk of cardiovascular disease who underwent hip surgery. The randomized controlled trial divided them into two groups, one of which got transfusions to maintain the hemoglobin levels above 10 g/dl while those in the other group weren’t given blood unless their hemoglobin fell below 8 g/dl. There were no statistically significant differences between the groups for mortality in the hospital or in terms of functional measures. Yet the amount of blood transfused in the 10 g/dl group was three times that of the 8 g/dl group. “We’re beginning to accumulate evidence that in most settings we can use less blood,” says Jeffrey Carson, chief of general internal medicine at Rutgers Robert Wood Johnson Medical School, who led the study. “But we still need a lot more trials, especially in high-risk groups, and to see whether we can safely go lower than 7 to 8 g/dl.”
RICHARD BENJAMIN, CHIEF MEDICAL OFFICER OF THE AMERICAN RED CROSS, which supplies approximately 40% of the nation’s blood supply, was among many experts who had expected that blood use would rise as baby boomers aged and the number of surgical procedures and cancer treatments soared. In fact, though, after the steep rise that peaked late in the past decade, hospitals have been using less blood. In 2011, 13.8 million units of whole blood and red blood cells were transfused—8.2% less than in 2008. And while Benjamin believes some of that drop can be explained by economic pressures that led fewer patients to opt for elective surgery, blood management programs have also begun to make an impact.
Stanford University Medical Center, for example, which launched its program in 2010, has cut its red blood use from 45,000 units a year to 35,000 units. Goodnough gives much of the credit to a simple tool in the electronic health record system, an alert that reminds physicians to think twice before ordering transfusions for stable, nonbleeding patients with hemoglobin levels of 7 g/dl or above. The alert includes a link to medical society guidelines for transfusions, and asks physicians who do order blood to document a reason for transfusion. “There’s no question that the tool is having a substantial impact,” Goodnough says.
Many hospitals don’t have the leadership or resources to develop such programs, and in some cases blood providers have supported the services of Hannon’s Strategic Healthcare Group for their hospital clients. But money’s yet another issue. “Most hospitals think blood management is a good idea, but they want absolute certainty that it will result in cost reductions,” says James AuBuchon, president of Puget Sound Blood Center and past president of the AABB. Of the 40 hospitals in the Seattle region that the blood center serves, only two have formal blood management programs.
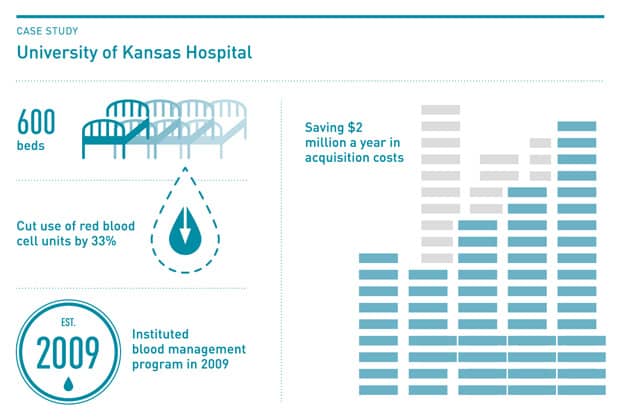
But transfusions are one of hospitals’ highest costs, and during the past decade, the average price of a unit of blood has risen from $100 to $200. Using less blood often does result in substantial savings. At the 600-bed University of Kansas Hospital, for example, a targeted program established in 2009 has cut its use of red blood cell units by a third, saving $2 million a year in blood acquisition costs, says Lowell Tilzer, the hospital’s chair of pathology and laboratory medicine. And despite physician worries about safety, the hospital’s mortality index has improved during the past couple of years, Tilzer says.
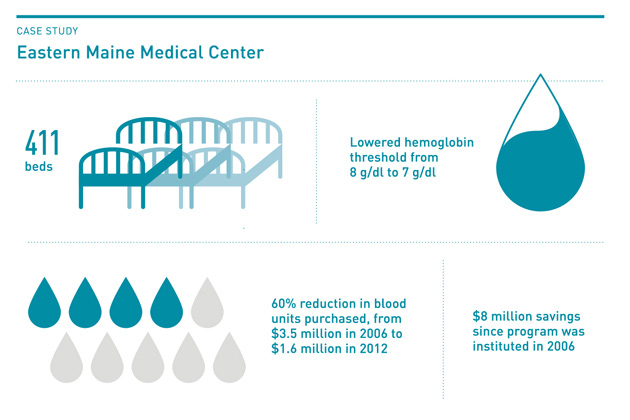
”There’s a lot of work to do in terms of education and changing physician practices and hospital systems so the care is uniform,” says Irwin Gross, a pathologist who led the effort to launch a comprehensive bloodless surgery program at the 411-bed Eastern Maine Medical Center in Bangor in 2006. Since the program started, the hospital’s annual expenditures on blood have plunged from $3.5 million a year to $1.6 million in 2012. That’s all the more impressive considering that the hospital lowered its hemoglobin threshold for transfusions for stable patients only marginally, from 8 g/dl to 7 g/dl. “Our threshold was conservative to begin with,” Gross says. He emphasizes that the program is “not just about a threshold number, but a host of interventions that start before the patient is even admitted to the hospital.”
FOR NOW, EFFORTS BY HOSPITALS to use less blood are voluntary. In 2011, the Joint Commission, the leading accreditation group for hospitals, issued seven voluntary measures to help hospitals manage their blood supplies. Although no one is collecting data on adherence to the guidelines, some people see regulation as inevitable. “It’s likely that within the next two to three years hospitals will have to show they have the policies and procedures of a blood management program,” says Mark Zawadsky, an orthopedic surgeon at MedStar Georgetown University Hospital in Washington, D.C.
Three years ago, Zawadsky led the establishment of the first bloodless surgery center for Jehovah’s Witnesses in the D.C. area, and the program has since been expanded to cover all patients at the hospital. The electronic health records system now incorporates a transfusion threshold of 7.5 g/dl, smaller blood samples are taken, and an anemia management program is being phased in. There’s also a new emphasis on using blood clotting drugs and blood salvage techniques in operating rooms.
Before the program, the hospital averaged 16,000 transfusions annually. That number has decreased by more than 10% during the past two years, saving the hospital more than $1 million. “What we’re finding,” Zawadsky says, “is that bloodless medicine is better medicine.”
Dossier
“Transfusion Medicine,” The Lancet, May 24, 2013. A comprehensive three-part series penned by various research experts that looks at the impact of innovations in patient blood management on the use of blood products, transfusion-free alternatives, and better ways to manage the blood supply to meet increasing global demand.
www.sabm.org. The website for the Society for the Advancement of Blood Management is a leading source of current research, evidence-based practices and other knowledge concerning blood management.
Stay on the frontiers of medicine
Related Stories
- An Imperfect 10
Often ridiculed, ICD-10 may relieve some diagnostic and billing headaches. But implementation will bring complications.
- Defined: Helium Cliff
An impending helium shortage could greatly raise the price of helium, an element used to chill MRI scanners.
- What Lies Beneath
A young woman’s uncomfortable experience in the hospital and the memory it forged.